*This is a medical informational site only and and should be treated as such. It is not intended nor should be used for self diagnosis and treatment. If you have any medical conditions or concerns, you should always see your medical provider for a proper and thorough clinical work-up and evaluation. We do not endorse or favor any specific commercial product or company. Trade, proprietary, or company names appearing in this document are used only because they are considered necessary in the context of the information provided. If a product is not mentioned, the omission does not mean or imply that the product is unsatisfactory.
Carpal Tunnel Syndrome
What is carpal tunnel syndrome?
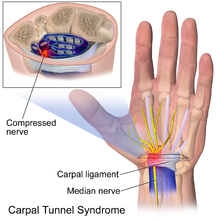
Carpal tunnel syndrome occurs when the median nerve, which runs from the forearm into the palm of the hand, becomes pressed or squeezed at the wrist. The median nerve controls sensations to the palm side of the thumb and fingers (although not the little finger), as well as impulses to some small muscles in the hand that allow the fingers and thumb to move. The carpal tunnel - a narrow, rigid passageway of ligament and bones at the base of the hand - houses the median nerve and tendons. Sometimes, thickening from irritated tendons or other swelling narrows the tunnel and causes the median nerve to be compressed. The result may be pain, weakness, or numbness in the hand and wrist, radiating up the arm. Although painful sensations may indicate other conditions, carpal tunnel syndrome is the most common and widely known of the entrapment neuropathies in which the body's peripheral nerves are compressed or traumatized.
Symptoms
Symptoms usually start gradually, with frequent burning, tingling, or itching numbness in the palm of the hand and the fingers, especially the thumb and the index and middle fingers. Some carpal tunnel sufferers say their fingers feel useless and swollen, even though little or no swelling is apparent. The symptoms often first appear in one or both hands during the night, since many people sleep with flexed wrists. A person with carpal tunnel syndrome may wake up feeling the need to "shake out" the hand or wrist. As symptoms worsen, people might feel tingling during the day. Decreased grip strength may make it difficult to form a fist, grasp small objects, or perform other manual tasks. In chronic and/or untreated cases, the muscles at the base of the thumb may waste away. Some people are unable to tell between hot and cold by touch.
Causes
Carpal tunnel syndrome is often the result of a combination of factors that increase pressure on the median nerve and tendons in the carpal tunnel, rather than a problem with the nerve itself. Most likely the disorder is due to a congenital predisposition - the carpal tunnel is simply smaller in some people than in others. Other contributing factors include trauma or injury to the wrist that cause swelling, such as sprain or fracture; overactivity of the pituitary gland; hypothyroidism; rheumatoid arthritis; mechanical problems in the wrist joint; work stress; repeated use of vibrating hand tools; fluid retention during pregnancy or menopause; or the development of a cyst or tumor in the canal. In some cases no cause can be identified.
There is little clinical data to prove whether repetitive and forceful movements of the hand and wrist during work or leisure activities can cause carpal tunnel syndrome. Other disorders such as bursitis and tendonitis have been associated with repeated motions performed in the course of normal work or other activities.. Writer's cramp may also be brought on by repetitive activity.
Risk of developing carpal tunnel syndrome
Women are three times more likely than men to develop carpal tunnel syndrome, perhaps because the carpal tunnel itself may be smaller in women than in men. The dominant hand is usually affected first and produces the most severe pain. Persons with diabetes or other metabolic disorders that directly affect the body's nerves and make them more susceptible to compression are also at high risk. Carpal tunnel syndrome usually occurs only in adults.
The risk of developing carpal tunnel syndrome is not confined to people in a single industry or job, but is especially common in those performing assembly line work - manufacturing, sewing, finishing, cleaning, and meat, poultry, or fish packing. In fact, carpal tunnel syndrome is three times more common among assemblers than among data-entry personnel.
Diagnosis
Early diagnosis and treatment are important to avoid permanent damage to the median nerve. A physical examination of the hands, arms, shoulders, and neck can help determine if the patient's complaints are related to daily activities or to an underlying disorder, and can rule out other painful conditions that mimic carpal tunnel syndrome. The wrist is examined for tenderness, swelling, warmth, and discoloration. Each finger should be tested for sensation, and the muscles at the base of the hand should be examined for strength and signs of atrophy. Routine laboratory tests and X-rays can reveal diabetes, arthritis, and fractures.
Physicians can use specific tests to try to produce the symptoms of carpal tunnel syndrome. In the Tinel test, the doctor taps on or presses on the median nerve in the patient's wrist. The test is positive when tingling in the fingers or a resultant shock-like sensation occurs. The Phalen, or wrist-flexion, test involves having the patient hold his or her forearms upright by pointing the fingers down and pressing the backs of the hands together. The presence of carpal tunnel syndrome is suggested if one or more symptoms, such as tingling or increasing numbness, is felt in the fingers within 1 minute. Doctors may also ask patients to try to make a movement that brings on symptoms.
Often it is necessary to confirm the diagnosis by use of electrodiagnostic tests. In a nerve conduction study, electrodes are placed on the hand and wrist. Small electric shocks are applied and the speed with which nerves transmit impulses is measured. In electromyography, a fine needle is inserted into a muscle; electrical activity viewed on a screen can determine the severity of damage to the median nerve. Ultrasound imaging can show impaired movement of the median nerve. Magnetic resonance imaging (MRI) can show the anatomy of the wrist but to date has not been especially useful in diagnosing carpal tunnel syndrome.
How is carpal tunnel syndrome treated?
Treatments for carpal tunnel syndrome should begin as early as possible, under a doctor's direction. Underlying causes such as diabetes or arthritis should be treated first. Initial treatment generally involves resting the affected hand and wrist for at least 2 weeks, avoiding activities that may worsen symptoms, and immobilizing the wrist in a splint to avoid further damage from twisting or bending. If there is inflammation, applying cool packs can help reduce swelling.
Non-surgical treatments
Drugs - In special circumstances, various drugs can ease the pain and swelling associated with carpal tunnel syndrome. Nonsteroidal anti-inflammatory drugs, such as aspirin, ibuprofen, and other nonprescription pain relievers, may ease symptoms that have been present for a short time or have been caused by strenuous activity. Orally administered diuretics ("water pills") can decrease swelling. Corticosteroids (such as prednisone) or the drug lidocaine can be injected directly into the wrist or taken by mouth (in the case of prednisone) to relieve pressure on the median nerve and provide immediate, temporary relief to persons with mild or intermittent symptoms. (Caution: persons with diabetes and those who may be predisposed to diabetes should note that prolonged use of corticosteroids can make it difficult to regulate insulin levels. Corticosteroids should not be taken without a doctor's prescription.) Additionally, some studies show that vitamin B6 (pyridoxine) supplements may ease the symptoms of carpal tunnel syndrome.
Exercise - Stretching and strengthening exercises can be helpful in people whose symptoms have abated. These exercises may be supervised by a physical therapist, who is trained to use exercises to treat physical impairments, or an occupational therapist, trained in evaluating people with physical impairments and helping them build skills to improve their health and well-being.
Alternative therapies - Acupuncture and chiropractic care have benefited some patients but their effectiveness remains unproved. An exception is yoga, which has been shown to reduce pain and improve grip strength among some patients with carpal tunnel syndrome.
Surgery
Carpal tunnel release is one of the most common surgical procedures in the United States. Generally recommended if symptoms last for 6 months, surgery involves severing the band of tissue around the wrist to reduce pressure on the median nerve. Surgery is done under local anesthesia and does not require an overnight hospital stay. Many patients require surgery on both hands.
The following are types of carpal tunnel release surgery:
Open release surgery, the traditional procedure used to correct carpal tunnel syndrome, consists of making an incision up to 2 inches in the wrist and then cutting the carpal ligament to enlarge the carpal tunnel. The procedure is generally done under local anesthesia on an outpatient basis, unless there are unusual medical considerations.
Endoscopic surgery may allow faster functional recovery and less postoperative discomfort than traditional open release surgery. The surgeon makes two incisions (about ½ inch each) in the wrist and palm, inserts a camera attached to a tube, observes the tissue on a screen, and cuts the carpal ligament (the tissue that holds joints together). This two-portal endoscopic surgery, generally performed under local anesthesia, is effective and minimizes scarring and scar tenderness, if any. Single portal endoscopic surgery for carpal tunnel syndrome is also available and can result in less post-operative pain and a minimal scar. It generally allows individuals to resume some normal activities in a short period of time.
Although symptoms may be relieved immediately after surgery, full recovery from carpal tunnel surgery can take months. Some patients may have infection, nerve damage, stiffness, and pain at the scar. Occasionally the wrist loses strength because the carpal ligament is cut. Patients should undergo physical therapy after surgery to restore wrist strength. Some patients may need to adjust job duties or even change jobs after recovery from surgery.
Recurrence of carpal tunnel syndrome following treatment is rare. The majority of patients recover completely.
How can carpal tunnel syndrome be prevented?
At the workplace, workers can do on-the-job conditioning, perform stretching exercises, take frequent rest breaks, wear splints to keep wrists straight, and use correct posture and wrist position. Wearing fingerless gloves can help keep hands warm and flexible. Workstations, tools and tool handles, and tasks can be redesigned to enable the worker's wrist to maintain a natural position during work. Jobs can be rotated among workers. Employers can develop programs in ergonomics, the process of adapting workplace conditions and job demands to the capabilities of workers. However, research has not conclusively shown that these workplace changes prevent the occurrence of carpal tunnel syndrome.
Research
Scientists are studying the factors that lead to long-lasting neuropathies, and how the affected nerves are related to symptoms of pain, numbness, and functional loss. Researchers also are examining biomechanical stresses that contribute to the nerve damage responsible for symptoms of carpal tunnel syndrome in order to better understand, treat, and prevent this ailment. By quantifying the distinct biomechanical pressures from fluid and anatomical structures, researchers are finding ways to limit or prevent carpal tunnel syndrome in the workplace and decrease other costly and disabling occupational illnesses.
Scientists are also investigating the effects of acupuncture on pain, loss of median nerve function, and changes in the brain associated with carpal tunnel syndrome. In addition, a randomized clinical trial designed to evaluate the effectiveness of osteopathic manipulative treatment in conjunction with standard medical care is underway. Evaluations of these therapies and other therapies will help to tailor patient treatment programs.
**National Institute of Neurological Disorders and Stroke
National Institutes of Health
Bethesda, MD 20892
***http://drgregorybennettmd.weebly.com/
Presbyopia
What is presbyopia?
Presbyopia is a common type of vision disorder that occurs as you age. It is often referred to as the aging eye condition. Presbyopia results in the inability to focus up close, a problem associated with refraction in the eye.
Can I have presbyopia and another type of refractive error at the same time?
Yes. It is common to have presbyopia and another type of refractive error at the same time. There are several other types of refractive errors: myopia (nearsightedness), hyperopia (farsightedness), and astigmatism.
An individual may have one type of refractive error in one eye and a different type of refractive error in the other.
What is refraction?
Refraction is the bending of light as it passes through one object to another. Vision occurs when light rays are bent (refracted) by the cornea and lens. The light is then focused directly on the retina, which is a light-sensitive tissue at the back of the eye. The retina converts the light-rays into messages that are sent through the optic nerve to the brain. The brain interprets these messages into the images we see.
Causes and Risk Factors
How does presbyopia occur?
Presbyopia happens naturally in people as they age. The eye is not able to focus light directly on to the retina due to the hardening of the natural lens. Aging also affects muscle fibers around the lens making it harder for the eye to focus on up close objects. The ineffective lens causes light to focus behind the retina, causing poor vision for objects that are up close.
When you are younger, the lens of the eye is soft and flexible, allowing the tiny muscles inside the eye to easily reshape the lens to focus on close and distant objects.
Who is at risk for presbyopia?
Anyone over the age of 35 is at risk for developing presbyopia. Everyone experiences some loss of focusing power for near objects as they age, but some will notice this more than others.
Symptoms and Detection
What are the signs and symptoms of presbyopia?
Some of the signs and symptoms of myopia include:
- Hard time reading small print
- Having to hold reading material farther than arm's distance
- Problems seeing objects that are close to you
- Headaches
- Eyestrain
If you experience any of these symptoms you may want to visit an eye care professional for a comprehensive dilated eye examination. If you wear glasses or contact lenses and still have these issues, a new prescription might be needed.
How is presbyopia diagnosed?
Presbyopia can be found during a comprehensive dilated eye exam. If you notice any changes in your vision, you should visit an eye care professional. Exams are recommended more often after the age 40 to check for age-related conditions.
Treatment
How is presbyopia corrected?
Eyeglasses are the simplest and safest means of correcting presbyopia. Eyeglasses for presbyopia have higher focusing power in the lower portion of the lens. This allows you to read through the lower portion of the lens and see properly at distant through the upper portion of the lens. It is also possible to purchase reading eyeglasses. These types of glasses do not require a prescription and can help with reading vision. In the past, some doctors told patients with presbyopia that they were not good candidates for multifocal lenses. Although fitting presbyopic patients with multifocal contacts is more complicated than fitting people without it, it’s a good option for many. Multifocal contact lenses, can also correct for both distance and near vision problems. Some patients do well with a different therapeutic approach called monovision. Rather than correcting both eyes for both distance and near vision problems, monovision corrects one eye for distance vision and one eye for near vision. Basically the brain learns to ignore the image that’s not in focus. This can be accomplished with contact lenses or through Lasik surgery, which reshapes the cornea. However, if someone is considering an irreversible process like Lasik, it’s important to test monovision first with contact lenses. Another option for some under certain circumstances is Lens Replacement. As the eye ages, the lens may develop cataracts, or cloudiness. Eye surgeons correct the problem by replacing the lens. Now some of these intraocular lenses can also correct for presbyopia.
*National Eye Institute
Diabetic Retinopathy
What is diabetic eye disease?
Diabetic eye disease refers to a group of eye problems that people with diabetes may face as a complication of diabetes. All can cause severe vision loss or even blindness.
Diabetic eye disease may include:
- Diabetic retinopathy—damage to the blood vessels in the retina.
- Cataract—clouding of the eye's lens. Cataracts develop at an earlier age in people with diabetes.
- Glaucoma—increase in fluid pressure inside the eye that leads to optic nerve damage and loss of vision. A person with diabetes is nearly twice as likely to get glaucoma as other adults.
What is diabetic retinopathy?
Diabetic retinopathy is the most common diabetic eye disease and a leading cause of blindness in American adults. It is caused by changes in the blood vessels of the retina.
In some people with diabetic retinopathy, blood vessels may swell and leak fluid. In other people, abnormal new blood vessels grow on the surface of the retina. The retina is the light-sensitive tissue at the back of the eye. A healthy retina is necessary for good vision.
If you have diabetic retinopathy, at first you may not notice changes to your vision. But over time, diabetic retinopathy can get worse and cause vision loss. Diabetic retinopathy usually affects both eyes.
What are the stages of diabetic retinopathy?
Diabetic retinopathy has four stages:
- Mild Nonproliferative Retinopathy. At this earliest stage, microaneurysms occur. They are small areas of balloon-like swelling in the retina's tiny blood vessels.
- Moderate Nonproliferative Retinopathy. As the disease progresses, some blood vessels that nourish the retina are blocked
- Severe Nonproliferative Retinopathy. Many more blood vessels are blocked, depriving several areas of the retina with their blood supply. These areas of the retina send signals to the body to grow new blood vessels for nourishment.
- Proliferative Retinopathy. At this advanced stage, the signals sent by the retina for nourishment trigger the growth of new blood vessels. This condition is called proliferative retinopathy. These new blood vessels are abnormal and fragile. They grow along the retina and along the surface of the clear, vitreous gel that fills the inside of the eye. By themselves, these blood vessels do not cause symptoms or vision loss. However, they have thin, fragile walls. If they leak blood, severe vision loss and even blindness can result.
Causes and Risk Factors
How does diabetic retinopathy cause vision loss?
Blood vessels damaged from diabetic retinopathy can cause vision loss in two ways:
- Fragile, abnormal blood vessels can develop and leak blood into the center of the eye, blurring vision. This is proliferative retinopathy and is the fourth and most advanced stage of the disease.
- Fluid can leak into the center of the macula, the part of the eye where sharp, straight-ahead vision occurs. The fluid makes the macula swell, blurring vision. This condition is called macular edema. It can occur at any stage of diabetic retinopathy, although it is more likely to occur as the disease progresses. About half of the people with proliferative retinopathy also have macular edema
(below) Normal Vision and the same scene viewed by a person with diabetic retinopathy
Normal vision
Same scene viewed by a person with diabetic
retinopathy
Who is at risk for diabetic retinopathy?
All people with diabetes--both type 1 and type 2--are at risk. That's why everyone with diabetes should get a comprehensive dilated eye exam at least once a year. The longer someone has diabetes, the more likely he or she will get diabetic retinopathy. Between 40 to 45 percent of Americans diagnosed with diabetes have some stage of diabetic retinopathy. If you have diabetic retinopathy, your doctor can recommend treatment to help prevent its progression.
During pregnancy, diabetic retinopathy may be a problem for women with diabetes. To protect vision, every pregnant woman with diabetes should have a comprehensive dilated eye exam as soon as possible. Your doctor may recommend additional exams during your pregnancy.
What can I do to protect my vision?
If you have diabetes get a comprehensive dilated eye exam at least once a year and remember:
- Proliferative retinopathy can develop without symptoms. At this advanced stage, you are at high risk for vision loss.
- Macular edema can develop without symptoms at any of the four stages of diabetic retinopathy.
- You can develop both proliferative retinopathy and macular edema and still see fine. However, you are at high risk for vision loss.
- Your eye care professional can tell if you have macular edema or any stage of diabetic retinopathy. Whether or not you have symptoms, early detection and timely treatment can prevent vision loss.
If you have diabetic retinopathy, you may need an eye exam more often. People with proliferative retinopathy can reduce their risk of blindness by 95 percent with timely treatment and appropriate follow-up care. The Diabetes Control and Complications Trial (DCCT) showed that better control of blood sugar levels slows the onset and progression of retinopathy. The people with diabetes who kept their blood sugar levels as close to normal as possible also had much less kidney and nerve disease. Better control also reduces the need for sight-saving laser surgery.
This level of blood sugar control may not be best for everyone, including some elderly patients, children under age 13, or people with heart disease. Be sure to ask your doctor if such a control program is right for you.
Other studies have shown that controlling elevated blood pressure and cholesterol can reduce the risk of vision loss. Controlling these will help your overall health as well as help protect your vision.
Symptoms and Detection
Does diabetic retinopathy have any symptoms?
Often there are no symptoms in the early stages of the disease, nor is there any pain. Don't wait for symptoms. Be sure to have a comprehensive dilated eye exam at least once a year.
Blurred vision may occur when the macula—the part of the retina that provides sharp central vision—swells from leaking fluid. This condition is called macular edema.
If new blood vessels grow on the surface of the retina, they can bleed into the eye and block vision.
What are the symptoms of proliferative retinopathy if bleeding occurs?
At first, you will see a few specks of blood, or spots, "floating" in your vision. If spots occur, see your eye care professional as soon as possible. You may need treatment before more serious bleeding occurs. Hemorrhages tend to happen more than once, often during sleep.
Sometimes, without treatment, the spots clear, and you will see better. However, bleeding can reoccur and cause severely blurred vision. You need to be examined by your eye care professional at the first sign of blurred vision, before more bleeding occurs.
If left untreated, proliferative retinopathy can cause severe vision loss and even blindness. Also, the earlier you receive treatment, the more likely treatment will be effective.
How are diabetic retinopathy and macular edema detected?
Diabetic retinopathy and macular edema are detected during a comprehensive eye exam that includes:
- Visual acuity test. This eye chart test measures how well you see at various distances.
- Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. This allows the eye care professional to see more of the inside of your eyes to check for signs of the disease. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry. An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
Your eye care professional checks your retina for early signs of the disease, including:
- Leaking blood vessels.
- Retinal swelling (macular edema).
- Pale, fatty deposits on the retina--signs of leaking blood vessels.
- Damaged nerve tissue.
- Any changes to the blood vessels.
If your eye care professional believes you need treatment for macular edema, he or she may suggest a fluorescein angiogram. In this test, a special dye is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your retina. The test allows your eye care professional to identify any leaking blood vessels and recommend treatment.
Treatment
How is diabetic retinopathy treated?
During the first three stages of diabetic retinopathy, no treatment is needed, unless you have macular edema. To prevent progression of diabetic retinopathy, people with diabetes should control their levels of blood sugar, blood pressure, and blood cholesterol.
Proliferative retinopathy is treated with laser surgery. This procedure is called scatter laser treatment. Scatter laser treatment helps to shrink the abnormal blood vessels. Your doctor places 1,000 to 2,000 laser burns in the areas of the retina away from the macula, causing the abnormal blood vessels to shrink. Because a high number of laser burns are necessary, two or more sessions usually are required to complete treatment. Although you may notice some loss of your side vision, scatter laser treatment can save the rest of your sight. Scatter laser treatment may slightly reduce your color vision and night vision.
Scatter laser treatment works better before the fragile, new blood vessels have started to bleed. That is why it is important to have regular, comprehensive dilated eye exams. Even if bleeding has started, scatter laser treatment may still be possible, depending on the amount of bleeding.
If the bleeding is severe, you may need a surgical procedure called a vitrectomy. During a vitrectomy, blood is removed from the center of your eye.
How is a macular edema treated?
Macular edema is treated with laser surgery. This procedure is called focal laser treatment. Your doctor places up to several hundred small laser burns in the areas of retinal leakage surrounding the macula. These burns slow the leakage of fluid and reduce the amount of fluid in the retina. The surgery is usually completed in one session. Further treatment may be needed.
A patient may need focal laser surgery more than once to control the leaking fluid. If you have macular edema in both eyes and require laser surgery, generally only one eye will be treated at a time, usually several weeks apart.
Focal laser treatment stabilizes vision. In fact, focal laser treatment reduces the risk of vision loss by 50 percent. In a small number of cases, if vision is lost, it can be improved. Contact your eye care professional if you have vision loss.
NEI research found that prompt treatment of macular edema with the drug Lucentis, with or without laser treatment, resulted in better vision than laser treatment alone or steroid injections. When injected into the eye, Lucentis, and two other similar drugs, Avastin or Aylea, reduce fluid leakage and interfere with the growth of new blood vessels in the retina.
What happens during laser treatment?
Both focal and scatter laser treatment are performed in your doctor's office or eye clinic. Before the surgery, your doctor will dilate your pupil and apply drops to numb the eye. The area behind your eye also may be numbed to prevent discomfort.
The lights in the office will be dim. As you sit facing the laser machine, your doctor will hold a special lens to your eye. During the procedure, you may see flashes of light. These flashes eventually may create a stinging sensation that can be uncomfortable. You will need someone to drive you home after surgery. Because your pupil will remain dilated for a few hours, you should bring a pair of sunglasses.
For the rest of the day, your vision will probably be a little blurry. If your eye hurts, your doctor can suggest treatment.
Laser surgery and appropriate follow-up care can reduce the risk of blindness by 90 percent. However, laser surgery often cannot restore vision that has already been lost. That is why finding diabetic retinopathy early is the best way to prevent vision loss.
What is a vitrectomy?
If you have a lot of blood in the center of the eye (vitreous gel), you may need a vitrectomy to restore your sight. If you need vitrectomies in both eyes, they are usually done several weeks apart.
A vitrectomy is performed under either local or general anesthesia. Your doctor makes a tiny incision in your eye. Next, a small instrument is used to remove the vitreous gel that is clouded with blood. The vitreous gel is replaced with a salt solution. Because the vitreous gel is mostly water, you will notice no change between the salt solution and the original vitreous gel.
You will probably be able to return home after the vitrectomy. Some people stay in the hospital overnight. Your eye will be red and sensitive. You will need to wear an eye patch for a few days or weeks to protect your eye. You also will need to use medicated eyedrops to protect against infection.
Are scatter laser treatment and vitrectomy effective in treating proliferative retinopathy?
Yes. Both treatments are very effective in reducing vision loss. People with proliferative retinopathy have less than a five percent chance of becoming blind within five years when they get timely and appropriate treatment. Although both treatments have high success rates, they do not cure diabetic retinopathy.
Once you have proliferative retinopathy, you always will be at risk for new bleeding. You may need treatment more than once to protect your sight.
What can I do if I already have lost some vision from diabetic retinopathy?
If you have lost some sight from diabetic retinopathy, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments. A nearby school of medicine or optometry may provide low vision services.
Current Research
What research is being done?
The National Eye Institute (NEI) is conducting and supporting research that seeks better ways to detect, treat, and prevent vision loss in people with diabetes. This research is conducted through studies in the laboratory and with patients.
For example, researchers are studying drugs that may stop the retina from sending signals to the body to grow new blood vessels. Someday, these drugs may help people control their diabetic retinopathy and reduce the need for laser surgery.
*National Eye Institute
Floaters
What are floaters?
Floaters are little "cobwebs" or specks that float about in your field of vision. They are small, dark, shadowy shapes that can look like spots, thread-like strands, or squiggly lines. They move as your eyes move and seem to dart away when you try to look at them directly. They do not follow your eye movements precisely, and usually drift when your eyes stop moving.
Most people have floaters and learn to ignore them; they are usually not noticed until they become numerous or more prominent. Floaters can become apparent when looking at something bright, such as white paper or a blue sky.
Frequently Asked Questions about Floaters
Floaters and Retinal Detachment
Sometimes a section of the vitreous pulls the fine fibers away from the retina all at once, rather than gradually, causing many new floaters to appear suddenly. This is called a vitreous detachment, which in most cases is not sight-threatening and requires no treatment.
However, a sudden increase in floaters, possibly accompanied by light flashes or peripheral (side) vision loss, could indicate a retinal detachment. A retinal detachment occurs when any part of the retina, the eye's light-sensitive tissue, is lifted or pulled from its normal position at the back wall of the eye.
A retinal detachment is a serious condition and should always be considered an emergency. If left untreated, it can lead to permanent visual impairment within two or three days or even blindness in the eye.
Those who experience a sudden increase in floaters, flashes of light in peripheral vision, or a loss of peripheral vision should have an eye care professional examine their eyes as soon as possible.
Causes and Risk Factors
What causes floaters?
Floaters occur when the vitreous, a gel-like substance that fills about 80 percent of the eye and helps it maintain a round shape, slowly shrinks.
As the vitreous shrinks, it becomes somewhat stringy, and the strands can cast tiny shadows on the retina. These are floaters. In most cases, floaters are part of the natural aging process and simply an annoyance. They can be distracting at first, but eventually tend to "settle" at the bottom of the eye, becoming less bothersome. They usually settle below the line of sight and do not go away completely.
However, there are other, more serious causes of floaters, including infection, inflammation (uveitis), hemorrhaging, retinal tears, and injury to the eye.
Who is at risk for floaters?
Floaters are more likely to develop as we age and are more common in people who are very nearsighted, have diabetes, or who have had a cataract operation.
Symptoms and Detection
Floaters are little "cobwebs" or specks that float about in your field of vision. They are small, dark, shadowy shapes that can look like spots, thread-like strands, or squiggly lines. They move as your eyes move and seem to dart away when you try to look at them directly. They do not follow your eye movements precisely, and usually drift when your eyes stop moving.
Treatment
How are floaters treated?
For people who have floaters that are simply annoying, no treatment is recommended.
On rare occasions, floaters can be so dense and numerous that they significantly affect vision. In these cases, a vitrectomy, a surgical procedure that removes floaters from the vitreous, may be needed.
A vitrectomy removes the vitreous gel, along with its floating debris, from the eye. The vitreous is replaced with a salt solution. Because the vitreous is mostly water, you will not notice any change between the salt solution and the original vitreous.
This operation carries significant risks to sight because of possible complications, which include retinal detachment, retinal tears, and cataract. Most eye surgeons are reluctant to recommend this surgery unless the floaters seriously interfere with vision.
*National Eye Institute
31 Center Drive MSC 2510
Bethesda, MD 20892-2510
Gallstone Disease
What are gallstones?
Gallstones are hard particles that develop in the gallbladder. The gallbladder is a small, pear-shaped organ located in the upper right abdomen—the area between the chest and hips—below the liver.
Gallstones can range in size from a grain of sand to a golf ball. The gallbladder can develop a single large gallstone, hundreds of tiny stones, or both small and large stones. Gallstones can cause sudden pain in the upper right abdomen. This pain, called a gallbladder attack or biliary colic, occurs when gallstones block the ducts of the biliary tract.
What is the biliary tract?
The biliary tract consists of the gallbladder and the bile ducts. The bile ducts carry bile and other digestive enzymes from the liver and pancreas to the duodenum—the first part of the small intestine. The liver produces bile—a fluid that carries toxins and waste products out of the body and helps the body digest fats and the fat-soluble vitamins A, D, E, and K. Bile mostly consists of cholesterol, bile salts, and bilirubin. Bilirubin, a reddish-yellow substance, forms when hemoglobin from red blood cells breaks down. Most bilirubin is excreted through bile.
Illustration of the biliary system, with the liver, gallbladder, duodenum,
pancreatic duct, common bile duct, pancreas, cystic duct, and hepatic ducts labeled.
The biliary tract
The bile ducts of the biliary tract include the hepatic ducts, the common bile duct, the pancreatic duct, and the cystic duct. The gallbladder stores bile. Eating signals the gallbladder to contract and empty bile through the cystic duct and common bile duct into the duodenum to mix with food.
What causes gallstones?
Imbalances in the substances that make up bile cause gallstones. Gallstones may form if bile contains too much cholesterol, too much bilirubin, or not enough bile salts. Scientists do not fully understand why these imbalances occur. Gallstones also may form if the gallbladder does not empty completely or often enough.
The two types of gallstones are cholesterol and pigment stones:
- Cholesterol stones, usually yellow-green in color, consist primarily of hardened cholesterol. In the United States, more than 80 percent of gallstones are cholesterol stones.1
- Pigment stones, dark in color, are made of bilirubin.
Who is at risk for gallstones?
Certain people have a higher risk of developing gallstones than others: 2
- Women are more likely to develop gallstones than men. Extra estrogen can increase cholesterol levels in bile and decrease gallbladder contractions, which may cause gallstones to form. Women may have extra estrogen due to pregnancy, hormone replacement therapy, or birth control pills.
- People over age 40 are more likely to develop gallstones than younger people.
- People with a family history of gallstones have a higher risk.
- American Indians have genetic factors that increase the amount of cholesterol in their bile. In fact, American Indians have the highest rate of gallstones in the United States—almost 65 percent of women and 30 percent of men have gallstones.
- Mexican Americans are at higher risk of developing gallstones.
Other factors that affect a person’s risk of gallstones include: 2
- Obesity. People who are obese, especially women, have increased risk of developing gallstones. Obesity increases the amount of cholesterol in bile, which can cause stone formation.
- Rapid weight loss. As the body breaks down fat during prolonged fasting and rapid weight loss, the liver secretes extra cholesterol into bile. Rapid weight loss can also prevent the gallbladder from emptying properly. Low-calorie diets and bariatric surgery—surgery that limits the amount of food a person can eat or digest—lead to rapid weight loss and increased risk of gallstones.
- Diet. Research suggests diets high in calories and refined carbohydrates and low in fiber increase the risk of gallstones. Refined carbohydrates are grains processed to remove bran and germ, which contain nutrients and fiber. Examples of refined carbohydrates include white bread and white rice.
- Certain intestinal diseases. Diseases that affect normal absorption of nutrients, such as Crohn’s disease, are associated with gallstones.
- Metabolic syndrome, diabetes, and insulin resistance. These conditions increase the risk of gallstones. Metabolic syndrome also increases the risk of gallstone complications. Metabolic syndrome is a group of traits and medical conditions linked to being overweight or obese that puts people at risk for heart disease and type 2 diabetes. *You can read more about these conditions in Insulin Resistance and Prediabetes at www.diabetes.niddk.nih.gov.
Pigment stones tend to develop in people who have:
- cirrhosis—a condition in which the liver slowly deteriorates and malfunctions due to chronic, or long lasting, injury
- infections in the bile ducts
- severe hemolytic anemias—conditions in which red blood cells are continuously broken down, such as sickle cell anemia
What are the symptoms and complications of gallstones?
Many people with gallstones do not have symptoms. Gallstones that do not cause symptoms are called asymptomatic, or silent, gallstones. Silent gallstones do not interfere with the function of the gallbladder, liver, or pancreas.
If gallstones block the bile ducts, pressure increases in the gallbladder, causing a gallbladder attack. The pain usually lasts from 1 to several hours.1 Gallbladder attacks often follow heavy meals, and they usually occur in the evening or during the night.
Gallbladder attacks usually stop when gallstones move and no longer block the bile ducts. However, if any of the bile ducts remain blocked for more than a few hours, complications can occur. Complications include inflammation, or swelling, of the gallbladder and severe damage or infection of the gallbladder, bile ducts, or liver.
A gallstone that becomes lodged in the common bile duct near the duodenum and blocks the pancreatic duct can cause gallstone pancreatitis—inflammation of the pancreas.
Left untreated, blockages of the bile ducts or pancreatic duct can be fatal.
When should a person talk with a health care provider about gallstones?
People who think they have had a gallbladder attack should notify their health care provider. Although these attacks usually resolve as gallstones move, complications can develop if the bile ducts remain blocked.
People with any of the following symptoms during or after a gallbladder attack should see a health care provider immediately:
- abdominal pain lasting more than 5 hours
- nausea and vomiting
- fever—even a low-grade fever—or chills
- yellowish color of the skin or whites of the eyes, called jaundice
- tea-colored urine and light-colored stools
These symptoms may be signs of serious infection or inflammation of the gallbladder, liver, or pancreas.
How are gallstones diagnosed?
A health care provider will usually order an ultrasound exam to diagnose gallstones. Other imaging tests may also be used.
- Ultrasound exam. Ultrasound uses a device, called a transducer that bounces safe, painless sound waves off organs to create an image of their structure. A specially trained technician performs the procedure in a health care provider’s office, outpatient center, or hospital, and a radiologist—a doctor who specializes in medical imaging—interprets the images. Anesthesia is not needed. If gallstones are present, they will be visible in the image. Ultrasound is the most accurate method to detect gallstones.
Computerized tomography (CT) scan. A CT scan is an x ray that produces pictures of the body. A CT scan may include the injection of a special dye, called contrast medium. CT scans use a combination of x rays and computer technology to create three-dimensional (3-D) images. CT scans require the person to lie on a table that slides into a tunnel-shaped device where the x rays are taken. An x-ray technician performs the procedure in an outpatient center or hospital, and a radiologist interprets the images. Anesthesia is not needed. CT scans can show gallstones or complications, such as infection and blockage of the gallbladder or bile ducts. However, CT scans can miss gallstones that are present.
- Magnetic resonance imaging (MRI). MRI machines use radio waves and magnets to produce detailed pictures of the body’s internal organs and soft tissues without using x rays. A specially trained technician performs the procedure in an outpatient center or hospital, and a radiologist interprets the images. Anesthesia is not needed, though people with a fear of confined spaces may receive light sedation. An MRI may include the injection of contrast medium. With most MRI machines, the person lies on a table that slides into a tunnel-shaped device that may be open ended or closed at one end; some newer machines allow the person to lie in a more open space. MRIs can show gallstones in the ducts of the biliary system.
- Cholescintigraphy. Cholescintigraphy—also called a hydroxyl iminodiacetic acid scan, HIDA scan, or hepatobiliary scan—uses an unharmful radioactive material to produce pictures of the biliary system. In cholescintigraphy, the person lies on an exam table and a health care provider injects a small amount of unharmful radioactive material into a vein in the person’s arm. The health care provider may also inject a substance that causes the gallbladder to contract. A special camera takes pictures of the radioactive material as it moves through the biliary system. A specially trained technician performs the procedure in an outpatient center or hospital and a radiologist interprets the images. Anesthesia is not needed. Cholescintigraphy is used to diagnose abnormal contractions of the gallbladder or obstruction of the bile ducts.
- Endoscopic retrograde cholangiopancreatography (ERCP). ERCP uses an x ray to look into the bile and pancreatic ducts. After lightly sedating the person, the health care provider inserts an endoscope—a small, ‑flexible tube with a light and a camera on the end—through the mouth into the duodenum and bile ducts. The endoscope is connected to a computer and video monitor. The health care provider injects contrast medium through the tube into the bile ducts, which makes the ducts show up on the monitor. The health care provider performs the procedure in an outpatient center or hospital. ERCP helps the health care provider locate the affected bile duct and the gallstone. The stone is captured in a tiny basket attached to the endoscope and removed. This test is more invasive than other tests and is used selectively.
Health care providers also use blood tests to look for signs of infection or inflammation of the bile ducts, gallbladder, pancreas, or liver. A blood test involves drawing blood at a health care provider’s office or commercial facility and sending the sample to a lab for analysis.
Gallstone symptoms may be similar to those of other conditions, such as appendicitis, ulcers, pancreatitis, and gastroesophageal reflux disease. Sometimes, silent gallstones are found when a person does not have any symptoms. For example, a health care provider may notice gallstones when performing ultrasound for a different reason.
How are gallstones treated?
If gallstones are not causing symptoms, treatment is usually not needed. However, if a person has a gallbladder attack or other symptoms, a health care provider will usually recommend treatment. A person may be referred to a gastroenterologist—a doctor who specializes in digestive diseases—for treatment. If a person has had one gallbladder attack, more episodes will likely follow.
The usual treatment for gallstones is surgery to remove the gallbladder. If a person cannot undergo surgery, nonsurgical treatments may be used to dissolve cholesterol gallstones. A health care provider may use ERCP to remove stones in people who cannot undergo surgery or to remove stones from the common bile duct in people who are about to have gallbladder removal surgery.
Surgery
Surgery to remove the gallbladder, called cholecystectomy, is one of the most common operations performed on adults in the United States. The gallbladder is not an essential organ, which means a person can live normally without a gallbladder. Once the gallbladder is removed, bile flows out of the liver through the hepatic and common bile ducts and directly into the duodenum, instead of being stored in the gallbladder.
Surgeons perform two types of cholecystectomy:
- Laparoscopic cholecystectomy. In a laparoscopic cholecystectomy, the surgeon makes several tiny incisions in the abdomen and inserts a laparoscope—a thin tube with a tiny video camera attached. The camera sends a magnified image from inside the body to a video monitor, giving the surgeon a close-up view of organs and tissues. While watching the monitor, the surgeon uses instruments to carefully separate the gallbladder from the liver, bile ducts, and other structures. Then the surgeon removes the gallbladder through one of the small incisions. Patients usually receive general anesthesia. Most cholecystectomies are performed with laparoscopy. Many laparoscopic cholecystectomies are performed on an outpatient basis, meaning the person is able to go home the same day. Normal physical activity can usually be resumed in about a week.
- Open cholecystectomy. An open cholecystectomy is performed when the gallbladder is severely inflamed, infected, or scarred from other operations. In most of these cases, open cholecystectomy is planned from the start. However, a surgeon may perform an open cholecystectomy when problems occur during a laparoscopic cholecystectomy. In these cases, the surgeon must switch to open cholecystectomy as a safety measure for the patient. To perform an open cholecystectomy, the surgeon creates an incision about 4 to 6 inches long in the abdomen to remove the gallbladder.4 Patients usually receive general anesthesia. Recovery from open cholecystectomy may require some people to stay in the hospital for up to a week. Normal physical activity can usually be resumed after about a month.3
A small number of people have softer and more frequent stools after gallbladder removal because bile flows into the duodenum more often. Changes in bowel habits are usually temporary; however, they should be discussed with a health care provider.
Though complications from gallbladder surgery are rare, the most common complication is injury to the bile ducts. An injured common bile duct can leak bile and cause a painful and possibly dangerous infection. One or more additional operations may be needed to repair the bile ducts. Bile duct injuries occur in less than 1 percent of cholecystectomies.5
Nonsurgical Treatments for Cholesterol Gallstones
Nonsurgical treatments are used only in special situations, such as when a person with cholesterol stones has a serious medical condition that prevents surgery. Gallstones often recur within 5 years after nonsurgical treatment. 6
Two types of nonsurgical treatments can be used to dissolve cholesterol gallstones:
- Oral dissolution therapy. Ursodiol (Actigall) and chenodiol (Chenix) are medications that contain bile acids that can dissolve gallstones. These medications are most effective in dissolving small cholesterol stones. Months or years of treatment may be needed to dissolve all stones.
- Shock wave lithotripsy. A machine called a lithotripter is used to crush the gallstone. The lithotripter generates shock waves that pass through the person’s body to break the gallstone into smaller pieces. This procedure is used only rarely and may be used along with ursodiol.
Eating, Diet, and Nutrition
Factors related to eating, diet, and nutrition that increase the risk of gallstones include:
- obesity
- rapid weight loss
- diets high in calories and refined carbohydrates and low in fiber
People can decrease their risk of gallstones by maintaining a healthy weight through proper diet and nutrition. Ursodiol can help prevent gallstones in people who rapidly lose weight through low-calorie diets or bariatric surgery. People should talk with their health care provider or dietitian about what diet is right for them.
Points to Remember
- Gallstones are hard particles that develop in the gallbladder.
- Imbalances in the substances that make up bile cause gallstones. Gallstones may form if bile contains too much cholesterol, too much bilirubin, or not enough bile salts. Scientists do not fully understand why these imbalances occur.
- Women, people over age 40, people with a family history of gallstones, American Indians, and Mexican Americans have a higher risk of developing gallstones.
- Many people with gallstones do not have symptoms. Gallstones that do not cause symptoms are called asymptomatic, or silent, gallstones.
- If gallstones block the bile ducts, pressure increases in the gallbladder, causing a gallbladder attack.
- Gallbladder attacks often follow heavy meals, and they usually occur in the evening or during the night.
- Gallstone symptoms may be similar to those of other conditions.
- If gallstones are not causing symptoms, treatment is usually not needed. However, if a person has a gallbladder attack or other symptoms, a health care provider will usually recommend treatment.
- The usual treatment for gallstones is surgery to remove the gallbladder. If a person cannot undergo surgery, nonsurgical treatments may be used to dissolve cholesterol gallstones. A health care provider may use endoscopic retrograde cholangiopancreatography (ERCP) to remove stones in people who cannot undergo surgery or to remove stones from the common bile duct in people who are about to have gallbladder removal surgery.
- The gallbladder is not an essential organ, which means a person can live normally without a gallbladder. Once the gallbladder is removed, bile ‑flows out of the liver through the hepatic and common bile ducts and directly into the duodenum, instead of being stored in the gallbladder.
References
1. Heuman DM. Cholelithiasis. Medscape website. http://emedicine.medscape.com/article/175667-overview#showall.leaving site icon Updated May 13, 2013. Accessed July 23, 2013.
2. Stinton LM, Shaffer EA. Epidemiology of gallbladder disease: cholelithiasis and cancer. Gut and Liver. 2012;6(2):172–187.
3. Sherwinter DA. Laparoscopic cholecystectomy. Medscape website. http://emedicine.medscape.com/article/1582292-overview.leaving site icon Updated May 10, 2013. Accessed July 23, 2013.
4. Hope WW. Open cholecystectomy. Medscape website. http://emedicine.medscape.com/article/1582261-overview.leaving site icon Updated January 8, 2013. Accessed July 23, 2013.
5. Sahajpal AK, Chow SC, Dixon E, Greig PD, Gallinger S, Wei AC. Bile duct injuries associated with laparoscopic cholecystectomy: timing of repair and long-term outcomes. Archives of Surgery. 2010;145(8):757–763.
6. Portincasa P, Ciaula AD, Bonfrate L, Wang DQ. Therapy of gallstone disease: what it was, what it is, what it will be. World Journal of Gastrointestinal Pharmacology and Therapeutics. 2012;3(2):7–20.
Amblyopia
What is amblyopia?
The brain and the eyes work together to produce vision. The eye focuses light on the back part of the eye known as the retina. Cells of the retina then trigger nerve signals that travel along the optic nerves to the brain. Amblyopia is the medical term used when the vision of one eye is reduced because it fails to work properly with the brain. The eye itself looks normal, but for various reasons the brain favors the other eye. This condition is also sometimes called lazy eye.
How common is amblyopia?
Amblyopia is the most common cause of visual impairment among children, affecting approximately 2 to 3 out of every 100 children. Unless it is successfully treated in early childhood, amblyopia usually persists into adulthood. It is also the most common cause of monocular (one eye) visual impairment among young and middle-aged adults.
Cause
What causes amblyopia?
Amblyopia can result from any condition that prevents the eye from focusing clearly. Amblyopia can be caused by the misalignment of the two eyes—a condition called strabismus. With strabismus, the eyes can cross in (esotropia) or turn out (exotropia). Occasionally, amblyopia is caused by a clouding of the front part of the eye, a condition called cataract.
A common cause of amblyopia is the inability of one eye to focus as well as the other one. Amblyopia can occur when one eye is more nearsighted, more farsighted, or has more astigmatism. These terms refer to the ability of the eye to focus light on the retina. Farsightedness, or hyperopia, occurs when the distance from the front to the back of the eye is too short. Eyes that are farsighted tend to focus better at a distance but have more difficulty focusing on near objects. Nearsightedness, or myopia, occurs when the eye is too long from front to back. Eyes with nearsightedness tend to focus better on near objects. Eyes with astigmatism have difficulty focusing on far and near objects because of their irregular shape.
Treatment
How is amblyopia treated in children?
Treating amblyopia involves forcing the child to use the eye with weaker vision. There are two common ways to treat amblyopia:
Patching
An adhesive patch is worn over the stronger eye for weeks to months. This therapy forces the child to use the eye with amblyopia. Patching stimulates vision in the weaker eye and helps parts of the brain involved in vision develop more completely.
An NEI-funded study1 showed that patching the unaffected eye of children with moderate amblyopia for two hours daily works as well as patching for six hours daily. Shorter patching time can lead to better compliance with treatment and improved quality of life for children with amblyopia. However, a recent study2 showed that children whose amblyopia persists despite two hours of daily patching may improve if daily patching is extended to 6 hours.
Previously, eye care professionals thought that treating amblyopia would be of little benefit to older children. However, results from a nationwide clinical trial3 showed that many children from ages seven to 17 years old benefited from treatment for amblyopia. This study shows that age alone should not be used as a factor to decide whether or not to treat a child for amblyopia.
Atropine
A drop of a drug called atropine is placed in the stronger eye to temporarily blur vision so that the child will use the eye with amblyopia, especially when focusing on near objects. NEI-supported research4 has shown that atropine eye drops, when placed in the unaffected eye once a day, work as well as eye patching. Atropine eye drops are sometimes easier for parents and children to use.
Can amblyopia be treated in adults?
Studies are very limited at this time, and scientists don’t know the success rate for treating amblyopia in adults. During the first seven to ten years of life, the visual system develops rapidly. Important connections between the eye and the brain are created during this period of growth and development. Scientists are exploring whether treatment for amblyopia in adults can improve vision.
The National Eye Institute (NEI) is part of the National Institutes of Health (NIH) and is the Federal government's lead agency for vision research that leads to sight-saving treatments and plays a key role in reducing visual impairment and blindness.
Citations
1. Reduced Daily Eye Patching Effectively Treats Childhood's Most Common Eye Disorder. NEI press release. May 12, 2013.
2. Extended daily eye patching effective at treating stubborn amblyopia in children. NEI press release. September 23, 20133.
3. Older Children Can Benefit From Treatment For Childhood's Most Common Eye Disorder. NEI press release. April 11, 2005.
4. Eye Drops to Treat Childhood Eye Disorder Work As Well as Patching the Eye. NEI press release. March 13, 2002
*National Eye Institute
31 Center Drive MSC 2510
Bethesda, MD 20892-2510
(301) 496-5248
www.nei.nih.gov
ational Eye Institute
31 Center Drive MSC 2510
Bethesda, MD 20892-251
Common Allergens
*Some common seasonal and non-seasonal allergens and asthma irritants and preventive strategies that might help you avoid exposure to these substances during allergy season.
The information contained on this Web site is provided for educational and informational purposes only and shouldn't be used as a guide for diagnosing or treatment of any medical condition without the advice and supervision of your health care provider.
**Pollen
Ragweed Pollen

Ragweed and other weeds such as curly dock, lambs quarters, pigweed, plantain, sheep sorrel and sagebrush are some of the most prolific producers of pollen allergensDictionary of Environmental Health.
Although the ragweed pollen season runs from August to November, ragweed pollen levels usually peak in mid-September in many areas in the country.
In addition, pollen counts are highest between 5 - 10 AM and on dry, hot and windy days.
Preventive Strategies
- Avoid the outdoors between 5-10 AM. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Grass Pollen
As with tree pollen, grass pollen is regional as well as seasonal. In addition, grass pollen levels can be affected by temperature, time of day and rain.
Of the 1,200 species of grass that grow in North America, only a small percentage of these cause allergies. The most common grasses that can cause allergies are:
|
|
Preventive Strategies
Specifically:
- If you have a grass lawn, have someone else do the mowing. If you must mow the lawn yourself, wear a mask.
- Keep grass cut short.
- Choose ground covers that don't produce much pollen, such as Irish moss, bunch, and dichondra.
In General:
- Avoid the outdoors between 5-10 AM. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Tree Pollen
Trees can aggravate your allergy whether or not they are on your property, since trees release large amounts of pollen that can be distributed miles away from the original source.
Trees are the earliest pollen producers, releasing their pollen as early as January in the Southern states and as late as May or June in the Northern states.
Most allergies are specific to one type of tree such as:
|
|
|
or to the male cultivar of certain trees. The female of these species are totally pollen-free:
|
|
|
Some people, though, do show cross-reactivity among trees in the alder, beech, birch and oak family, and the juniper and cedar family.
Preventive Strategies
- If you buy trees for your yard, look for species that do not aggravate allergies such as crape myrtle, dogwood, fig, fir, palm, pear, plum, redbud and redwood trees or the female cultivars of ash, box elder, cottonwood, maple, palm, poplar or willow trees.
- Avoid the outdoors between 5-10 AM. Save outside activities for late afternoon or after a heavy rain, when pollen levels are lower.
- Keep windows in your home and car closed to lower exposure to pollen. To keep cool, use air conditioners and avoid using window and attic fans.
- Be aware that pollen can also be transported indoors on people and pets.
- Dry your clothes in an automatic dryer rather than hanging them outside. Otherwise pollen can collect on clothing and be carried indoors.
Dust Mites

Dust mites are tiny microscopic relatives of the spider and live on mattresses, bedding, upholstered furniture, carpets and curtains.
These tiny creatures feed on the flakes of skin that people and pets shed daily and they thrive in warm and humid environments.
No matter how clean a home is, dust mites cannot be totally eliminated. However, the number of mites can be reduced by following the suggestions below.
Preventive Strategies
- Use a dehumidifier or air conditioner to maintain relative humidity at about 50% or below.
- Encase your mattress and pillows in dust-proof or allergen impermeable covers (available from specialty supply mail order companies, bedding and some department stores).
- Wash all bedding and blankets once a week in hot water (at least 130 - 140°F) to kill dust mites. Non-washable bedding can be frozen overnight to kill dust mites.
- Replace wool or feathered bedding with synthetic materials and traditional stuffed animals with washable ones.
- If possible, replace wall-to-wall carpets in bedrooms with bare floors (linoleum, tile or wood) and remove fabric curtains and upholstered furniture.
- Use a damp mop or rag to remove dust. Never use a dry cloth since this just stirs up mite allergens.
- Use a vacuum cleaner with either a double-layered microfilter bag or a HEPA filter to trap allergens that pass through a vacuum's exhaust.
- Wear a mask while vacuuming to avoid inhaling allergens, and stay out of the vacuumed area for 20 minutes to allow any dust and allergens to settle after vacuuming.
Pets & Animals


Many people think animal allergies are caused by the fur or feathers of their pet. In fact, allergies are actually aggrevated by:
- proteins secreted by oil glands and shed as dander
- proteins in saliva (which stick to fur when animals lick themselves)
- aerosolized urine from rodents and guinea pigs
Keep in mind that you can sneeze with and without your pet being present. Although an animal may be out of sight, their allergens are not. This is because pet allergens are carried on very small particles. As a result pet allergens can remain circulatlng in the air and remain on carpets and furniture for weeks and months after a pet is gone. Allergens may also be present in public buildings, schools, etc. where there are no pets.
Preventive Strategies
- Remove pets from your home if possible.
- If pet removal is not possible, keep them out of bedrooms and confined to areas without carpets or upholstered furniture.
- If possible, bathe pets weekly to reduce the amount of allergens.
- Wear a dust mask and gloves when near rodents.
- After playing with your pet, wash your hands and clean your clothes to remove pet allergens.
- Avoid contact with soiled litter cages.
- Dust often with a damp cloth.
Mold

Several molds that grow both indoors and outdoors, produce allergenic substances. These allergens can be found in mold spores and other fungal structures (e.g. hyphae). There is no definite seasonal pattern to molds that grow indoors. However outdoor molds are seasonal, first appearing in early spring and thriving until the first frost.
Indoor molds are found in dark, warm, humid and musty environments such as damp basements, cellars, attics, bathrooms and laundry rooms. They are also found where fresh food is stored, in refrigerator drip trays, garbage pails, air conditioners and humidifiers.
Outdoor molds grow in moist shady areas. They are common in soil, decaying vegetation, compost piles, rotting wood and fallen leaves.
Preventive Strategies
- Use a dehumidifier or air conditioner to maintain relative humidity below 50% and keep temperatures cool.
- Vent bathrooms and clothes dryers to the outside, and run bathroom and kitchen vents while bathing and cooking.
- Regularly check faucets, pipes and ductwork for leaks.
- When first turning on home or car air conditioners, leave the room or drive with the windows open for several minutes to allow mold spores to disperse.
- Remove decaying debris from the yard, roof and gutters.
- Avoid raking leaves, mowing lawns or working with peat, mulch, hay or dead wood. If you must do yard work, wear a mask and avoid working on hot, humid days.
Cockroaches

Cockroaches are one of the most common and allergenic of indoor pests.
Recent studies have found a strong association between the presence of cockroaches and increases in the severity of asthma symptoms in individuals who are sensitive to cockroach allergens.
These pests are common even in the cleanest of crowded urban areas and older dwellings. They are found in all types of neighborhoods.
The proteins found in cockroach saliva are particularly allergenic but the body and droppings of cockroaches also contain allergenic proteins.
Preventive Strategies
- Keep food and garbage in closed, tight-lidded containers. Never leave food out in the kitchen.
- Do not leave out pet food or dirty food bowls.
- Eliminate water sources that attract these pests, such as leaky faucets and drain pipes.
- Mop the kitchen floor and wash countertops at least once a week.
- Plug up crevices around the house through which cockroaches can enter.
- Limit the spread of food around the house and especially keep food out of bedrooms.
- Use bait stations and other environmentally safe pesticides to reduce cockroach infestation.
**National Institute of Environmental Health Sciences 111 T.W. Alexander Drive, Research Triangle Park, NC USA 27709
Macular Degeneration
Age-related macular degeneration (AMD) is the major cause of severe vision loss in people over age 60. There is currently no cure, but in some cases the progression of the disease can be slowed or revered somewhat.
What is age-related macular degeneration?
Age-related macular degeneration (AMD) is a disease associated with aging that gradually destroys sharp, central vision. Central vision is needed for seeing objects clearly and for common daily tasks such as reading and driving.
AMD affects the macula, the part of the eye that allows you to see fine detail. AMD causes no pain.
In some cases, AMD advances so slowly that people notice little change in their vision. In others, the disease progresses faster and may lead to a loss of vision in both eyes. AMD is a leading cause of vision loss in Americans 60 years of age and older.
AMD occurs in two forms: wet and dry. 
Where is the macula?
The macula is located in the center of the retina, the light-sensitive tissue at the back of the eye. The retina instantly converts light, or an image, into electrical impulses. The retina then sends these impulses, or nerve signals, to the brain.
What is wet AMD?
Wet AMD occurs when abnormal blood vessels behind the retina start to grow under the macula. These new blood vessels tend to be very fragile and often leak blood and fluid. The blood and fluid raise the macula from its normal place at the back of the eye. Damage to the macula occurs rapidly.
With wet AMD, loss of central vision can occur quickly. Wet AMD is also known as advanced AMD. It does not have stages like dry AMD.
An early symptom of wet AMD is that straight lines appear wavy. If you notice this condition or other changes to your vision, contact your eye care professional at once. You need a comprehensive dilated eye exam.
What is dry AMD?
Dry AMD occurs when the light-sensitive cells in the macula slowly break down, gradually blurring central vision in the affected eye. As dry AMD gets worse, you may see a blurred spot in the center of your vision. Over time, as less of the macula functions, central vision is gradually lost in the affected eye.
The most common symptom of dry AMD is slightly blurred vision. You may have difficulty recognizing faces. You may need more light for reading and other tasks. Dry AMD generally affects both eyes, but vision can be lost in one eye while the other eye seems unaffected.
One of the most common early signs of dry AMD is drusen.
What are drusen?
Drusen are yellow deposits under the retina. They often are found in people over age 60. Your eye care professional can detect drusen during a comprehensive dilated eye exam.
Drusen alone do not usually cause vision loss. In fact, scientists are unclear about the connection between drusen and AMD. They do know that an increase in the size or number of drusen raises a person's risk of developing either advanced dry AMD or wet AMD. These changes can cause serious vision loss.
Dry AMD has three stages, all of which may occur in one or both eyes:
1. Early AMD. People with early AMD have either several small drusen or a few medium-sized drusen. At this stage, there are no symptoms and no vision loss.
2. Intermediate AMD. People with intermediate AMD have either many medium-sized drusen or one or more large drusen. Some people see a blurred spot in the center of their vision. More light may be needed for reading and other tasks.
3. Advanced Dry AMD. In addition to drusen, people with advanced dry AMD have a breakdown of light-sensitive cells and supporting tissue in the central retinal area. This breakdown can cause a blurred spot in the center of your vision. Over time, the blurred spot may get bigger and darker, taking more of your central vision. You may have difficulty reading or recognizing faces until they are very close to you.
If you have vision loss from dry AMD in one eye only, you may not notice any changes in your overall vision. With the other eye seeing clearly, you still can drive, read, and see fine details. You may notice changes in your vision only if AMD affects both eyes. If blurriness occurs in your vision, see an eye care professional for a comprehensive dilated eye exam.
Ninety percent of all people with AMD have this type. Scientists are still not sure what causes dry AMD.
Frequently Asked Questions about wet and dry AMD
Which is more common-the dry form or the wet form?
The dry form is much more common. More than 85 percent of all people with intermediate and advanced AMD combined have the dry form.
However, if only advanced AMD is considered, about two-thirds of patients have the wet form. Because almost all vision loss comes from advanced AMD, the wet form leads to significantly more vision loss than the dry form.
Can the dry form turn into the wet form?
Yes. All people who have the wet form had the dry form first.
The dry form can advance and cause vision loss without turning into the wet form. The dry form also can suddenly turn into the wet form, even during early stage AMD. There is no way to tell if or when the dry form will turn into the wet form.
The dry form has early and intermediate stages. Does the wet form have similar stages?
No. The wet form is considered advanced AMD.
Can advanced AMD be either the dry form or the wet form?
Yes. Both the wet form and the advanced dry form are considered advanced AMD. Vision loss occurs with either form. In most cases, only advanced AMD can cause vision loss.
People who have advanced AMD in one eye are at especially high risk of developing advanced AMD in the other eye.
Causes and Risk Factors
Who is at risk for AMD?
The greatest risk factor is age. Although AMD may occur during middle age, studies show that people over age 60 are clearly at greater risk than other age groups. For instance, a large study found that people in middle-age have about a 2 percent risk of getting AMD, but this risk increased to nearly 30 percent in those over age 75.
Other risk factors include:
Smoking. Smoking may increase the risk of AMD.
Obesity. Research studies suggest a link between obesity and the progression of early and intermediate stage AMD to advanced AMD.
Race. Whites are much more likely to lose vision from AMD than African Americans.
Family history. Those with immediate family members who have AMD are at a higher risk of developing the disease.
Gender. Women appear to be at greater risk than men.
Can my lifestyle make a difference?
Your lifestyle can play a role in reducing your risk of developing AMD.
Eat a healthy diet high in green leafy vegetables and fish.
Don't smoke.
Maintain normal blood pressure.
Watch your weight.
Exercise.
Symptoms and Detection
What are the symptoms?
Both dry and wet AMD cause no pain.
For dry AMD: the most common early sign is blurred vision. As fewer cells in the macula are able to function, people will see details less clearly in front of them, such as faces or words in a book. Often this blurred vision will go away in brighter light. If the loss of these light-sensing cells becomes great, people may see a small--but growing--blind spot in the middle of their field of vision.
For wet AMD: the classic early symptom is that straight lines appear crooked. This results when fluid from the leaking blood vessels gathers and lifts the macula, distorting vision. A small blind spot may also appear in wet AMD, resulting in loss of one's central vision.
How is AMD detected?
Your eye care professional may suspect AMD if you are over age 60 and have had recent changes in your central vision. To look for signs of the disease, he or she will use eye drops to dilate, or enlarge, your pupils. Dilating the pupils allows your eye care professional to view the back of the eye better.
AMD is detected during a comprehensive eye exam that includes:
1. Visual acuity test. This eye chart test measures how well you see at various distances.
2. Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of AMD and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
3. Tonometry. An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
Your eye care professional also may do other tests to learn more about the structure and health of your eye.
During an eye exam, you may be asked to look at an Amsler grid. The pattern of the grid resembles a checkerboard. You will cover one eye and stare at a black dot in the center of the grid. While staring at the dot, you may notice that the straight lines in the pattern appear wavy. You may notice that some of the lines are missing. These may be signs of AMD.
If your eye care professional believes you need treatment for wet AMD, he or she may suggest a fluorescein angiogram. In this test, a special dye is injected into your arm. Pictures are taken as the dye passes through the blood vessels in your retina. The test allows your eye care professional to identify any leaking blood vessels and recommend treatment.
Treatment
How is wet AMD treated?
Wet AMD can be treated with laser surgery, photodynamic therapy, and injections into the eye. None of these treatments is a cure for wet AMD. The disease and loss of vision may progress despite treatment.
1. Laser surgery. This procedure uses a laser to destroy the fragile, leaky blood vessels. A high energy beam of light is aimed directly onto the new blood vessels and destroys them, preventing further loss of vision. However, laser treatment may also destroy some surrounding healthy tissue and some vision. Only a small percentage of people with wet AMD can be treated with laser surgery. Laser surgery is more effective if the leaky blood vessels have developed away from the fovea, the central part of the macula. (See illustration at the beginning of this document.) Laser surgery is performed in a doctor's office or eye clinic.
The risk of new blood vessels developing after laser treatment is high. Repeated treatments may be necessary. In some cases, vision loss may progress despite repeated treatments.
2. Photodynamic therapy. A drug called verteporfin is injected into your arm. It travels throughout the body, including the new blood vessels in your eye. The drug tends to "stick" to the surface of new blood vessels. Next, a light is shined into your eye for about 90 seconds. The light activates the drug. The activated drug destroys the new blood vessels and leads to a slower rate of vision decline. Unlike laser surgery, this drug does not destroy surrounding healthy tissue. Because the drug is activated by light, you must avoid exposing your skin or eyes to direct sunlight or bright indoor light for five days after treatment.
Photodynamic therapy is relatively painless. It takes about 20 minutes and can be performed in a doctor's office.
Photodynamic therapy slows the rate of vision loss. It does not stop vision loss or restore vision in eyes already damaged by advanced AMD. Treatment results often are temporary. You may need to be treated again.
3. Injections. Wet AMD can now be treated with new drugs that are injected into the eye (anti-VEGF therapy). Abnormally high levels of a specific growth factor occur in eyes with wet AMD and promote the growth of abnormal new blood vessels. This drug treatment blocks the effects of the growth factor.
You will need multiple injections that may be given as often as monthly. The eye is numbed before each injection. After the injection, you will remain in the doctor's office for a while and your eye will be monitored. This drug treatment can help slow down vision loss from AMD and in some cases improve sight.
How is dry AMD treated?
Once dry AMD reaches the advanced stage, no form of treatment can prevent vision loss. However, treatment can delay and possibly prevent intermediate AMD from progressing to the advanced stage, in which vision loss occurs.
The National Eye Institute's Age-Related Eye Disease Study (AREDS) found that taking a specific high-dose formulation of antioxidants and zinc significantly reduces the risk of advanced AMD and its associated vision loss. Slowing AMD's progression from the intermediate stage to the advanced stage will save the vision of many people.
Watch Video on Treatment of AMD. Click on URL: http://www.youtube.com/watch?feature=player_detailpage&v=4qKz-CiI2Lw#t=76
Age-Related Eye Disease Study (AREDS)
What is the dosage of the AREDS formulation?
The specific daily amounts of antioxidants and zinc used by the study researchers were 500 milligrams of vitamin C, 400 International Units of vitamin E, 15 milligrams of beta-carotene (often labeled as equivalent to 25,000 International Units of vitamin A), 80 milligrams of zinc as zinc oxide, and two milligrams of copper as cupric oxide. Copper was added to the AREDS formulation containing zinc to prevent copper deficiency anemia, a condition associated with high levels of zinc intake.
Who should take the AREDS formulation?
People who are at high risk for developing advanced AMD should consider taking the formulation. You are at high risk for developing advanced AMD if you have either:
1. Intermediate AMD in one or both eyes.
OR
2. Advanced AMD (dry or wet) in one eye but not the other eye.
Your eye care professional can tell you if you have AMD, its stage, and your risk for developing the advanced form.
The AREDS formulation is not a cure for AMD. It will not restore vision already lost from the disease. However, it may delay the onset of advanced AMD. It may help people who are at high risk for developing advanced AMD keep their vision.
Can people with early stage AMD take the AREDS formulation to help prevent the disease from progressing to the intermediate stage?
There is no apparent need for those diagnosed with early stage AMD to take the AREDS formulation. The study did not find that the formulation provided a benefit to those with early stage AMD. If you have early stage AMD, a comprehensive dilated eye exam every year can help determine if the disease is progressing. If early stage AMD progresses to the intermediate stage, discuss taking the formulation with your doctor.
Can diet alone provide the same high levels of antioxidants and zinc as the AREDS formulation?
No. The high levels of vitamins and minerals are difficult to achieve from diet alone. However, previous studies have suggested that people who have diets rich in green leafy vegetables have a lower risk of developing AMD.
Can a daily multivitamin alone provide the same high levels of antioxidants and zinc as the AREDS formulation?
No. The formulation's levels of antioxidants and zinc are considerably higher than the amounts in any daily multivitamin.
If you are already taking daily multivitamins and your doctor suggests you take the high-dose AREDS formulation, be sure to review all your vitamin supplements with your doctor before you begin. Because multivitamins contain many important vitamins not found in the AREDS formulation, you may want to take a multivitamin along with the AREDS formulation. For example, people with osteoporosis need to be particularly concerned about taking vitamin D, which is not in the AREDS formulation.
How can I take care of my vision now that I have AMD?
Dry AMD. If you have dry AMD, you should have a comprehensive dilated eye exam at least once a year. Your eye care professional can monitor your condition and check for other eye diseases. Also, if you have intermediate AMD in one or both eyes, or advanced AMD in one eye only, your doctor may suggest that you take the AREDS formulation containing the high levels of antioxidants and zinc.
Because dry AMD can turn into wet AMD at any time, you should get an Amsler grid from your eye care professional. Use the grid every day to evaluate your vision for signs of wet AMD. This quick test works best for people who still have good central vision. Check each eye separately. Cover one eye and look at the grid. Then cover your other eye and look at the grid. If you detect any changes in the appearance of this grid or in your everyday vision while reading the newspaper or watching television, get a comprehensive dilated eye exam.
Wet AMD. If you have wet AMD and your doctor advises treatment, do not wait. After laser surgery or photodynamic therapy, you will need frequent eye exams to detect any recurrence of leaking blood vessels. Studies show that people who smoke have a greater risk of recurrence than those who don't. In addition, check your vision at home with the Amsler grid. If you detect any changes, schedule an eye exam immediately.
What can I do if I have already lost some vision from AMD?
If you have lost some sight from AMD, don't be afraid to use your eyes for reading, watching TV, and other routine activities. Normal use of your eyes will not cause further damage to your vision.
If you have lost some sight from AMD, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments. A nearby school of medicine or optometry may provide low vision services.
Current Research
What research is being done?
The National Eye Institute is conducting and supporting a number of studies to learn more about AMD. For example, scientists are:
Studying the possibility of transplanting healthy cells into a diseased retina.
Evaluating families with a history of AMD to understand genetic and hereditary factors that may cause the disease.
Looking at certain anti-inflammatory treatments for the wet form of AMD.
This research should provide better ways to detect, treat, and prevent vision loss in people with AMD.
National Eye Institute
31 Center Drive MSC 2510
Bethesda, MD 20892-2510
(301) 496-5248
www.nei.nih.gov
ational Eye Institute
31 Center Drive MSC 2510
Bethesda, MD 20892-251
Glaucoma
What is glaucoma?
Glaucoma is a group of diseases that can damage the eye's optic nerve and result in vision loss and blindness. Glaucoma occurs when the normal fluid pressure inside the eyes slowly rises. However, with early treatment, you can often protect your eyes against serious vision loss.
What is the optic nerve?
The optic nerve is a bundle of more than 1 million nerve fibers. It connects the retina to the brain. (See diagram below.) The retina is the light-sensitive tissue at the back of the eye. A healthy optic nerve is necessary for good vision.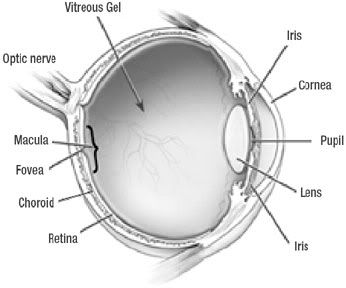
What are some other forms of glaucoma?
Open-angle glaucoma is the most common form. Some people have other types of the disease.
1. Low-tension or normal-tension glaucoma. Optic nerve damage and narrowed side vision occur in people with normal eye pressure. Lowering eye pressure at least 30 percent through medicines slows the disease in some people. Glaucoma may worsen in others despite low pressures.
A comprehensive medical history is important in identifying other potential risk factors, such as low blood pressure, that contribute to low-tension glaucoma. If no risk factors are identified, the treatment options for low-tension glaucoma are the same as for open-angle glaucoma.
2. Angle-closure glaucoma. The fluid at the front of the eye cannot reach the angle and leave the eye. The angle gets blocked by part of the iris. People with this type of glaucoma have a sudden increase in eye pressure. Symptoms include severe pain and nausea, as well as redness of the eye and blurred vision. If you have these symptoms, you need to seek treatment immediately.
This is a medical emergency. If your doctor is unavailable, go to the nearest hospital or clinic. Without treatment to improve the flow of fluid, the eye can become blind in as few as one or two days. Usually, prompt laser surgery and medicines can clear the blockage and protect sight.
3. Congenital glaucoma. Children are born with a defect in the angle of the eye that slows the normal drainage of fluid. These children usually have obvious symptoms, such as cloudy eyes, sensitivity to light, and excessive tearing. Conventional surgery typically is the suggested treatment, because medicines may have unknown effects in infants and be difficult to administer. Surgery is safe and effective. If surgery is done promptly, these children usually have an excellent chance of having good vision.
4. Secondary glaucomas. These can develop as complications of other medical conditions. These types of glaucomas are sometimes associated with eye surgery or advanced cataracts, eye injuries, certain eye tumors, or uveitis (eye inflammation). Pigmentary glaucoma occurs when pigment from the iris flakes off and blocks the meshwork, slowing fluid drainage. A severe form, called neovascular glaucoma, is linked to diabetes. Corticosteroid drugs used to treat eye inflammations and other diseases can trigger glaucoma in some people. Treatment includes medicines, laser surgery, or conventional surgery.
Causes and Risk Factors
How does open-angle glaucoma damage the optic nerve?
In the front of the eye is a space called the anterior chamber. A clear fluid flows continuously in and out of the chamber and nourishes nearby tissues. The fluid leaves the chamber at the open angle where the cornea and iris meet. (See diagram below.) When the fluid reaches the angle, it flows through a spongy meshwork, like a drain, and leaves the eye.
Sometimes, when the fluid reaches the angle, it passes too slowly through the meshwork drain. As the fluid builds up, the pressure inside the eye rises to a level that may damage the optic nerve. When the optic nerve is damaged from increased pressure, open-angle glaucoma--and vision loss--may result. That's why controlling pressure inside the eye is important.
Does increased eye pressure mean that I have glaucoma?
Not necessarily. Increased eye pressure means you are at risk for glaucoma, but does not mean you have the disease. A person has glaucoma only if the optic nerve is damaged. If you have increased eye pressure but no damage to the optic nerve, you do not have glaucoma. However, you are at risk. Follow the advice of your eye care professional.
Can I develop glaucoma if I have increased eye pressure?
Not necessarily. Not every person with increased eye pressure will develop glaucoma. Some people can tolerate higher eye pressure better than others. Also, a certain level of eye pressure may be high for one person but normal for another.
Whether you develop glaucoma depends on the level of pressure your optic nerve can tolerate without being damaged. This level is different for each person. That's why a comprehensive dilated eye exam is very important. It can help your eye care professional determine what level of eye pressure is normal for you.
Can I develop glaucoma without an increase in my eye pressure?
Yes. Glaucoma can develop without increased eye pressure. This form of glaucoma is called low-tension or normal-tension glaucoma. It is not as common as open-angle glaucoma.
Who is at risk for glaucoma?
Anyone can develop glaucoma. Some people are at higher risk than others. They include:
African Americans over age 40.
Everyone over age 60, especially Mexican Americans.
People with a family history of glaucoma.
Among African Americans, studies show that glaucoma is:
Five times more likely to occur in African Americans than in Caucasians.
About four times more likely to cause blindness in African Americans than in Caucasians.
Fifteen times more likely to cause blindness in African Americans between the ages of 45-64 than in Caucasians of the same age group.
A comprehensive dilated eye exam can reveal more risk factors, such as high eye pressure, thinness of the cornea, and abnormal optic nerve anatomy. In some people with certain combinations of these high-risk factors, medicines in the form of eyedrops reduce the risk of developing glaucoma by about half.
Medicare covers an annual comprehensive dilated eye exam for some people at high risk for glaucoma.
What can I do to protect my vision?
Studies have shown that the early detection and treatment of glaucoma, before it causes major vision loss, is the best way to control the disease. So, if you fall into one of the high-risk groups for the disease, make sure to have your eyes examined through dilated pupils every two years by an eye care professional.
If you are being treated for glaucoma, be sure to take your glaucoma medicine every day. See your eye care professional regularly.
You also can help protect the vision of family members and friends who may be at high risk for glaucoma--African Americans over age 40; everyone over age 60, especially Mexican Americans; and people with a family history of the disease. Encourage them to have a comprehensive dilated eye exam at least once every two years. Remember: Lowering eye pressure in glaucoma's early stages slows progression of the disease and helps save vision.
Symptoms and Detection
What are the symptoms of glaucoma?
At first, there are no symptoms. Vision stays normal, and there is no pain.
However, as the disease progresses, a person with glaucoma may notice his or her side vision gradually failing. That is, objects in front may still be seen clearly, but objects to the side may be missed.
As glaucoma remains untreated, people may miss objects to the side and out of the corner of their eye. Without treatment, people with glaucoma will slowly lose their peripheral (side) vision. They seem to be looking through a tunnel. Over time, straight-ahead vision may decrease until no vision remains.
Glaucoma can develop in one or both eyes.

Scene as viewed by person with glaucoma
How is glaucoma detected?
Glaucoma is detected through a comprehensive eye exam that includes:
1.Visual acuity test. This eye chart test measures how well you see at various distances. A tonometer measures pressure inside the eye to detect glaucoma.
2. Visual field test. This test measures your side (peripheral) vision. It helps your eye care professional tell if you have lost side vision, a sign of glaucoma.
3. Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
4. Tonometry. An instrument (right) measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
5. Pachymetry. A numbing drop is applied to your eye. Your eye care professional uses an ultrasonic wave instrument to measure the thickness of your cornea.
Treatment
Can glaucoma be treated?
Yes. Immediate treatment for early stage, open-angle glaucoma can delay progression of the disease. That's why early diagnosis is very important.
Glaucoma treatments include medicines, laser trabeculoplasty, conventional surgery, or a combination of any of these. While these treatments may save remaining vision, they do not improve sight already lost from glaucoma.
1. Medicines. Medicines, in the form of eyedrops or pills, are the most common early treatment for glaucoma. Some medicines cause the eye to make less fluid. Others lower pressure by helping fluid drain from the eye.
Before you begin glaucoma treatment, tell your eye care professional about other medicines you may be taking. Sometimes the drops can interfere with the way other medicines work.
Glaucoma medicines may be taken several times a day. Most people have no problems. However, some medicines can cause headaches or other side effects. For example, drops may cause stinging, burning, and redness in the eyes. Many drugs are available to treat glaucoma. If you have problems with one medicine, tell your eye care professional. Treatment with a different dose or a new drug may be possible.
Because glaucoma often has no symptoms, people may be tempted to stop taking, or may forget to take, their medicine. You need to use the drops or pills as long as they help control your eye pressure. Regular use is very important. Make sure your eye care professional shows you how to put the drops into your eye. See tips (hyperlink to "How should I use my glaucoma eyedrops?") on using your glaucoma eyedrops.
2. Laser trabeculoplasty. Laser trabeculoplasty helps fluid drain out of the eye. Your doctor may suggest this step at any time. In many cases, you need to keep taking glaucoma drugs after this procedure.
Laser trabeculoplasty is performed in your doctor's office or eye clinic. Before the surgery, numbing drops will be applied to your eye. As you sit facing the laser machine, your doctor will hold a special lens to your eye. A high-intensity beam of light is aimed at the lens and reflected onto the meshwork inside your eye. You may see flashes of bright green or red light. The laser makes several evenly spaced burns that stretch the drainage holes in the meshwork. This allows the fluid to drain better.
Like any surgery, laser surgery can cause side effects, such as inflammation. Your doctor may give you some drops to take home for any soreness or inflammation inside the eye. You need to make several follow-up visits to have your eye pressure monitored.
If you have glaucoma in both eyes, only one eye will be treated at a time. Laser treatments for each eye will be scheduled several days to several weeks apart.
Studies show that laser surgery is very good at reducing the pressure in some patients. However, its effects can wear off over time. Your doctor may suggest further treatment.
3. Conventional surgery. Conventional surgery makes a new opening for the fluid to leave the eye. (See diagram.) Your doctor may suggest this treatment at any time. Conventional surgery often is done after medicines and laser surgery have failed to control pressure.
Conventional surgery is performed in an eye clinic or hospital. Before the surgery, you will be given medicine to help you relax. Your doctor will make small injections around the eye to numb it. A small piece of tissue is removed to create a new channel for the fluid to drain from the eye.
For several weeks after the surgery, you must put drops in the eye to fight infection and inflammation. These drops will be different from those you may have been using before surgery.
As with laser surgery, conventional surgery is performed on one eye at a time. Usually the operations are four to six weeks apart. Conventional surgery is about 60 to 80 percent effective at lowering eye pressure. If the new drainage opening narrows, a second operation may be needed. Conventional surgery works best if you have not had previous eye surgery, such as a cataract operation.
In some instances, your vision may not be as good as it was before conventional surgery. Conventional surgery can cause side effects, including cataract, problems with the cornea, and inflammation or infection inside the eye. The buildup of fluid in the back of the eye may cause some patients to see shadows in their vision. If you have any of these problems, tell your doctor so a treatment plan can be developed.
Conventional surgery makes a new opening for the fluid to leave the eye.
Watch video on Glaucoma Treatment: Click on URL to watch: http://www.youtube.com/watch?feature=player_detailpage&v=X9NgArAMAQ8#t=13
How should I use my glaucoma eyedrops?
If eyedrops have been prescribed for treating your glaucoma, you need to use them properly and as instructed by your eye care professional. Proper use of your glaucoma medication can improve the medicine's effectiveness and reduce your risk of side effects. To properly apply your eyedrops, follow these steps:
First, wash your hands.
Hold the bottle upside down.
Tilt your head back.
Hold the bottle in one hand and place it as close as possible to the eye.
With the other hand, pull down your lower eyelid. This forms a pocket.
Place the prescribed number of drops into the lower eyelid pocket. If you are using more than one eyedrop, be sure to wait at least five minutes before applying the second eyedrop.
Close your eye OR press the lower lid lightly with your finger for at least one minute. Either of these steps keeps the drops in the eye and helps prevent the drops from draining into the tear duct, which can increase your risk of side effects
What can I do if I already have lost some vision from glaucoma?
If you have lost some sight from glaucoma, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision.
Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments. A nearby school of medicine or optometry may provide low vision services.
Current Research
What research is being done?
A large amount of research is being done in the U.S. to learn what causes glaucoma and to improve its diagnosis and treatment. For instance, the National Eye Institute (NEI) is funding a number of studies to find out what causes fluid pressure to increase in the eye. By learning more about this process, doctors may be able to find the exact cause of the disease and learn better how to prevent and treat it. The NEI also supports clinical trials of new drugs and surgical techniques that show promise against glaucoma
More Information
View Eye Health Organizations
Tips on Talking to Your Doctor
How to Find an Eye Care Professional
National Eye Institute
31 Center Drive MSC 2510
Bethesda, MD 20892-2510
(301) 496-5248
www.nei.nih.gov
Refractive Surgery
Reduce or eliminate the need for contacts and eyeglasses

The goal of refractive surgery, also called laser vision correction, is to correct nearsightedness, farsightedness, astigmatism and other eye conditions.
· LASIK and PRK: The most well-known types of refractive surgery -- laser-assisted in-situ keratomileusis LASIK and photorefractive keratectomy (PRK) -- both correct nearsightedness.
· CK: Conductive keratoplasty (CK) corrects farsightedness or presbyopia.
Which surgery is right for me?
You should first meet with an eye surgeon who can:
1. determine if you are a candidate for laser vision correction
2. assess your needs and eyeglasses or contact prescription
3. recommend which procedure is best for you.
Once you agree on the procedure, the surgeon should give instructions for everything from preparing for the surgery to recovery.
LASIK or Lasik (Laser-Assisted in situ Keratomileusis), commonly referred to as laser eye surgery, is a type of refractive surgery for the correction of myopia, hyperopia, and astigmatism. The LASIK surgery is performed by an ophthalmologist who uses a laser or microkeratome to reshape the eye's cornea in order to improve visual acuity.[1] For most patients, LASIK provides a permanent alternative to eyeglasses or contact lenses.[2] Major side effects include halos, starbursts, night-driving problems, keratoconus (corneal ectasia), and eye dryness.[3]
LASIK is most similar to another surgical corrective procedure, photorefractive keratectomy (PRK), and both represent advances over radial keratotomy in the surgical treatment of refractive errors of vision. For patients with moderate to high myopia or thin corneas which cannot be treated with LASIK and PRK, the phakic intraocular lens is an alternative
Watch video of LASIK ICL surgery implantation for high myopia. Click on URL to watch: http://www.youtube.com/watch?feature=player_profilepage&v=zYHUN1hx0Yo#t=81
Recognizing Cataracts
Watch for Vision Changes as You Age

As life goes on, we all start to notice certain changes that are a natural part of aging. Maybe our joints aren’t as flexible as before, or our hearing just isn’t what it used to be. Our vision, too, may be less sharp than it once was.
One cause of impaired eyesight later in life is cataracts. A cataract is a clouding of the lens in the eye. People with cataracts may notice cloudy vision or halos around lights when driving at night. If left untreated, cataracts can greatly limit vision. In fact, some people with severe cataracts may only be able to tell the difference between light and dark.
Cataracts are common in older adults. About half of all Americans will either have cataracts or have had cataract surgery by the time they reach age 80.
“I don’t usually think of cataract as an eye disease. In most cases, it’s simply a normal aging change of the eye,” says Dr. Rachel Bishop, an ophthalmologist (eye doctor) at NIH. “Typically, cataracts don’t cause damage to the eye the way most eye diseases do.”
Early symptoms of cataract can be improved with eyeglasses, brighter lighting, anti-glare sunglasses or magnifying lenses. If these steps don’t help, surgery is the only effective option for treatment. Surgery involves removing the cloudy lens and replacing it with a plastic lens.
Cataract procedures are among the most common surgeries performed in the United States. Most patients recover in just a few weeks, and many have improved eyesight after a few days. Recent advances have allowed doctors to tailor new lenses to patients and help reduce the need for eyeglasses after surgery.
The decision to have cataract surgery is a personal one that should be made between you and your doctor. Some experts advise that cataracts be removed only when vision loss interferes with your everyday activities, such as driving, reading or watching TV.
The best way to prevent or delay cataracts is to protect your eyes from harmful ultraviolet rays from the sun. Try wearing sunglasses or a hat with a brim. Researchers also believe that good nutrition can help reduce the risk of age-related cataract. They recommend eating plenty of green leafy vegetables, fruits, nuts and other healthy foods. Also, don’t smoke, because smoking may speed cataract development.
To screen for early signs of eye disease, Bishop recommends that everyone have a dilated eye exam at age 40, even if your vision seems fine. Once you’re in your 60s, a dilated eye exam is usually advised every year.
“Some people think reduced vision is just an unavoidable part of normal aging,” says Bishop. “It isn’t. If you notice your vision isn’t as good as it used to be, you should see your eye doctor.” Since many serious eye diseases have no early warning signs, it’s also important to make regular eye exams part of your standard health care routine. *NIH News in Health
(see more details below).
Cataract
A cataract is a clouding of the lens in the eye that affects vision. Most cataracts are related to aging. Cataracts are very common in older people. By age 80, more than half of all Americans either have a cataract or have had cataract surgery.
A cataract can occur in either or both eyes. It cannot spread from one eye to the other.
What is the lens?
The lens is a clear part of the eye that helps to focus light, or an image, on the retina. The retina is the light-sensitive tissue at the back of the eye.
In a normal eye, light passes through the transparent lens to the retina. Once it reaches the retina, light is changed into nerve signals that are sent to the brain.
The lens must be clear for the retina to receive a sharp image. If the lens is cloudy from a cataract, the image you see will be blurred.
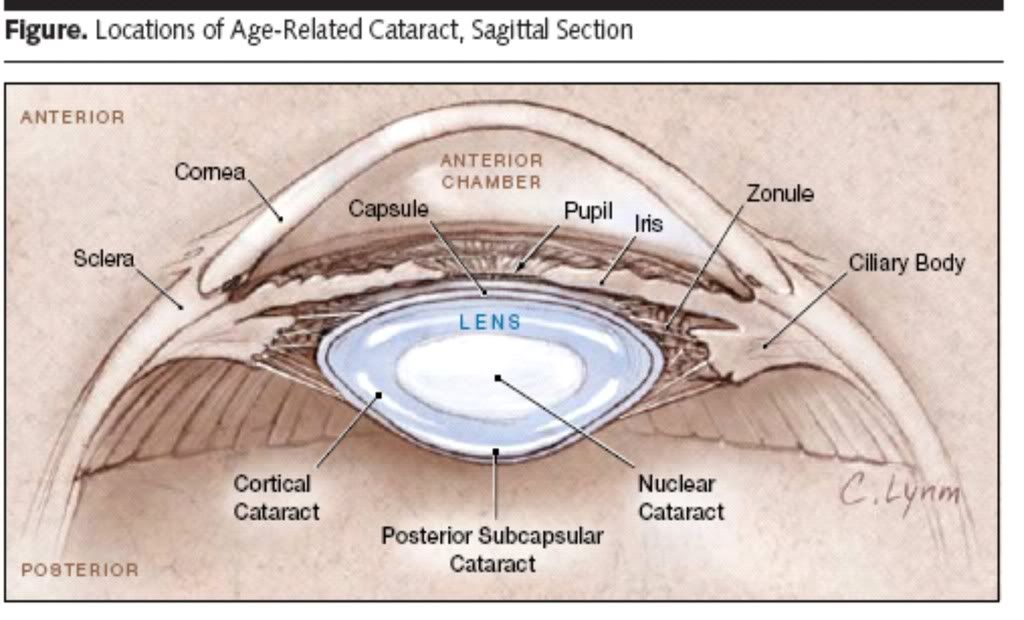
Are there other types of cataract?
Yes. Although most cataracts are related to aging, there are other types of cataract:
- Secondary cataract. Cataracts can form after surgery for other eye problems, such as glaucoma. Cataracts also can develop in people who have other health problems, such as diabetes. Cataracts are sometimes linked to steroid use.
- Traumatic cataract. Cataracts can develop after an eye injury, sometimes years later.
- Congenital cataract. Some babies are born with cataracts or develop them in childhood, often in both eyes. These cataracts may be so small that they do not affect vision. If they do, the lenses may need to be removed.
- Radiation cataract. Cataracts can develop after exposure to some types of radiation.
Causes and Risk Factors
What causes cataracts?
The lens lies behind the iris and the pupil. It works much like a camera lens. It focuses light onto the retina at the back of the eye, where an image is recorded. The lens also adjusts the eye's focus, letting us see things clearly both up close and far away. The lens is made of mostly water and protein. The protein is arranged in a precise way that keeps the lens clear and let’s light pass through it.
But as we age, some of the protein may clump together and start to cloud a small area of the lens. This is a cataract. Over time, the cataract may grow larger and cloud more of the lens, making it harder to see.
Researchers suspect that there are several causes of cataract, such as smoking and diabetes. Or, it may be that the protein in the lens just changes from the wear and tear it takes over the years.
How can cataracts affect my vision?
Age-related cataracts can affect your vision in two ways:
- Clumps of protein reduce the sharpness of the image reaching the retina.
The lens consists mostly of water and protein. When the protein clumps up, it clouds the lens and reduces the light that reaches the retina. The clouding may become severe enough to cause blurred vision. Most age-related cataracts develop from protein clumpings.
When a cataract is small, the cloudiness affects only a small part of the lens. You may not notice any changes in your vision. Cataracts tend to "grow" slowly, so vision gets worse gradually. Over time, the cloudy area in the lens may get larger, and the cataract may increase in size. Seeing may become more difficult. Your vision may get duller or blurrier.
- The clear lens slowly changes to a yellowish/brownish color, adding a brownish tint to vision.
As the clear lens slowly colors with age, your vision gradually may acquire a brownish shade. At first, the amount of tinting may be small and may not cause a vision problem. Over time, increased tinting may make it more difficult to read and perform other routine activities. This gradual change in the amount of tinting does not affect the sharpness of the image transmitted to the retina.
If you have advanced lens discoloration, you may not be able to identify blues and purples. You may be wearing what you believe to be a pair of black socks, only to find out from friends that you are wearing purple socks.
When are you most likely to have a cataract?
The term "age-related" is a little misleading. You don't have to be a senior citizen to get this type of cataract. In fact, people can have an age-related cataract in their 40s and 50s. But during middle age, most cataracts are small and do not affect vision. It is after age 60 that most cataracts steal vision.
Who is at risk for cataract?
The risk of cataract increases as you get older.
Other risk factors for cataract include:
- Certain diseases such as diabetes.
- Personal behavior such as smoking and alcohol use.
- The environment such as prolonged exposure to sunlight.
What can I do to protect my vision?
Wearing sunglasses and a hat with a brim to block ultraviolet sunlight may help to delay cataract. If you smoke, stop. Researchers also believe good nutrition can help reduce the risk of age-related cataract. They recommend eating green leafy vegetables, fruit, and other foods with antioxidants.
If you are age 60 or older, you should have a comprehensive dilated eye exam at least once every two years. In addition to cataract, your eye care professional can check for signs of age-related macular degeneration, glaucoma, and other vision disorders. Early treatment for many eye diseases may save your sight.
Symptoms and Detection
What are the symptoms of a cataract?
The most common symptoms of a cataract are:
- Cloudy or blurry vision.
- Colors seem faded.
- Glare. Headlights, lamps, or sunlight may appear too bright. A halo may appear around lights.
- Poor night vision.
- Double vision or multiple images in one eye. (This symptom may clear as the cataract gets larger.)
- Frequent prescription changes in your eyeglasses or contact lenses.
- These symptoms also can be a sign of other eye problems. If you have any of these symptoms, check with your eye care professional.
How is a cataract detected?
Cataract is detected through a comprehensive eye exam that includes:
- Visual acuity test. This eye chart test measures how well you see at various distances.
- Dilated eye exam. Drops are placed in your eyes to widen, or dilate, the pupils. Your eye care professional uses a special magnifying lens to examine your retina and optic nerve for signs of damage and other eye problems. After the exam, your close-up vision may remain blurred for several hours.
- Tonometry. An instrument measures the pressure inside the eye. Numbing drops may be applied to your eye for this test.
Your eye care professional also may do other tests to learn more about the structure and health of your eye.
Treatment
How is a cataract treated?
The symptoms of early cataract may be improved with new eyeglasses, brighter lighting, anti-glare sunglasses, or magnifying lenses. If these measures do not help, surgery is the only effective treatment.
Surgery involves removing the cloudy lens and replacing it with an artificial lens.
A cataract needs to be removed only when vision loss interferes with your everyday activities, such as driving, reading, or watching TV. You and your eye care professional can make this decision together.
Once you understand the benefits and risks of surgery, you can make an informed decision about whether cataract surgery is right for you.
In most cases, delaying cataract surgery will not cause long-term damage to your eye or make the surgery more difficult. You do not have to rush into surgery.
Sometimes a cataract should be removed even if it does not cause problems with your vision.
For example, a cataract should be removed if it prevents examination or treatment of another eye problem, such as age-related macular degeneration or diabetic retinopathy. If your eye care professional finds a cataract, you may not need cataract surgery for several years. In fact, you might never need cataract surgery. By having your vision tested regularly, you and your eye care professional can discuss if and when you might need treatment.
If you choose surgery, your eye care professional may refer you to a specialist to remove the cataract.
If you have cataracts in both eyes that require surgery, the surgery will be performed on each eye at separate times, usually four to eight weeks apart.
Many people who need cataract surgery also have other eye conditions, such as age-related macular degeneration or glaucoma. If you have other eye conditions in addition to cataract, talk with your doctor. Learn about the risks, benefits, alternatives, and expected results of cataract surgery.
What are the different types of cataract surgery?
There are two types of cataract surgery. Your doctor can explain the differences and help determine which is better for you:
- Phacoemulsification, or phaco. A small incision is made on the side of the cornea, the clear, dome-shaped surface that covers the front of the eye. Your doctor inserts a tiny probe into the eye. This device emits ultrasound waves that soften and break up the lens so that it can be removed by suction. Most cataract surgery today is done by phacoemulsification, also called "small incision cataract surgery."
- Extracapsular surgery. Your doctor makes a longer incision on the side of the cornea and removes the cloudy core of the lens in one piece. The rest of the lens is removed by suction.
After the natural lens has been removed, it often is replaced by an artificial lens, called an intraocular lens (IOL). An IOL is a clear, plastic lens that requires no care and becomes a permanent part of your eye. Light is focused clearly by the IOL onto the retina, improving your vision. You will not feel or see the new lens.
Some people cannot have an IOL. They may have another eye disease or have problems during surgery. For these patients, a soft contact lens, or glasses that provide high magnification, may be suggested.
What are the risks of cataract surgery?
As with any surgery, cataract surgery poses risks, such as infection and bleeding. Before cataract surgery, your doctor may ask you to temporarily stop taking certain medications that increase the risk of bleeding during surgery. After surgery, you must keep your eye clean, wash your hands before touching your eye, and use the prescribed medications to help minimize the risk of infection. Serious infection can result in loss of vision.
Cataract surgery slightly increases your risk of retinal detachment. Other eye disorders, such as high myopia (nearsightedness), can further increase your risk of retinal detachment after cataract surgery.
One sign of a retinal detachment is a sudden increase in flashes or floaters. Floaters are little "cobwebs" or specks that seem to float about in your field of vision. If you notice a sudden increase in floaters or flashes, see an eye care professional immediately. A retinal detachment is a medical emergency. If necessary, go to an emergency service or hospital. Your eye must be examined by an eye surgeon as soon as possible.
A retinal detachment causes no pain. Early treatment for retinal detachment often can prevent permanent loss of vision. The sooner you get treatment, the more likely you will regain good vision. Even if you are treated promptly, some vision may be lost.
Talk to your eye care professional about these risks. Make sure cataract surgery is right for you.
Is cataract surgery effective?
Cataract removal is one of the most common operations performed in the United States. It also is one of the safest and most effective types of surgery. In about 90 percent of cases, people who have cataract surgery have better vision afterward.
What happens before surgery?
A week or two before surgery, your doctor will do some tests. These tests may include measuring the curve of the cornea and the size and shape of your eye. This information helps your doctor choose the right type of IOL.
You may be asked not to eat or drink anything 12 hours before your surgery.
What happens during surgery?
At the hospital or eye clinic, drops will be put into your eye to dilate the pupil. The area around your eye will be washed and cleansed.
The operation usually lasts less than one hour and is almost painless. Many people choose to stay awake during surgery. Others may need to be put to sleep for a short time.
If you are awake, you will have an anesthetic to numb the nerves in and around your eye.
After the operation, a patch may be placed over your eye. You will rest for a while. Your medical team will watch for any problems, such as bleeding. Most people who have cataract surgery can go home the same day. You will need someone to drive you home.
What happens after surgery?
Itching and mild discomfort are normal after cataract surgery. Some fluid discharge is also common. Your eye may be sensitive to light and touch. If you have discomfort, your doctor can suggest treatment. After one or two days, moderate discomfort should disappear.
For a few days after surgery, your doctor may ask you to use eyedrops to help healing and decrease the risk of infection. Ask your doctor about how to use your eyedrops, how often to use them, and what effects they can have. You will need to wear an eye shield or eyeglasses to help protect your eye. Avoid rubbing or pressing on your eye.
When you are home, try not to bend from the waist to pick up objects on the floor. Do not lift any heavy objects. You can walk, climb stairs, and do light household chores.
In most cases, healing will be complete within eight weeks. Your doctor will schedule exams to check on your progress.
Can problems develop after surgery?
Problems after surgery are rare, but they can occur.
These problems can include:
- Infection
- Bleeding
- inflammation (pain, redness, swelling)
- loss of vision
- double vision
- high or low eye pressure
With prompt medical attention, these problems can usually be treated successfully.
Sometimes the eye tissue that encloses the IOL becomes cloudy and may blur your vision. This condition is called an after-cataract. An after-cataract can develop months or years after cataract surgery.
An after-cataract is treated with a laser. Your doctor uses a laser to make a tiny hole in the eye tissue behind the lens to let light pass through. This outpatient procedure is called a YAG laser capsulotomy. It is painless and rarely results in increased eye pressure or other eye problems. As a precaution, your doctor may give you eyedrops to lower your eye pressure before or after the procedure.
When will my vision be normal again?
You can return quickly to many everyday activities, but your vision may be blurry. The healing eye needs time to adjust so that it can focus properly with the other eye, especially if the other eye has a cataract. Ask your doctor when you can resume driving.
If you received an IOL, you may notice that colors are very bright. The IOL is clear, unlike your natural lens that may have had a yellowish/brownish tint. Within a few months after receiving an IOL, you will become used to improved color vision. Also, when your eye heals, you may need new glasses or contact lenses.
What can I do if I already have lost some vision from cataract?
If you have lost some sight from cataract or cataract surgery, ask your eye care professional about low vision services and devices that may help you make the most of your remaining vision. Ask for a referral to a specialist in low vision. Many community organizations and agencies offer information about low vision counseling, training, and other special services for people with visual impairments. A nearby school of medicine or optometry may provide low vision services.
Current Research
The National Eye Institute is conducting and supporting a number of studies focusing on factors associated with the development of age-related cataract. These studies include:
- The effect of sunlight exposure, which may be associated with an increased risk of cataract.
- Vitamin supplements, which have shown varying results in delaying the progression of cataract.
- Genetic studies, which show promise for better understanding cataract development.
National Eye Institute
31 Center Drive MSC 2510
Bethesda, MD 20892-2510
Dry Eye Disease
Dry eye occurs when the eye does not produce tears properly, or when the tears are not of the correct consistency and evaporate too quickly. In addition, inflammation of the surface of the eye may occur along with dry eye. If left untreated, this condition can lead to pain, ulcers, or scars on the cornea, and some loss of vision. However, permanent loss of vision from dry eye is uncommon. Dry eye can make it more difficult to perform some activities, such as using a computer or reading for an extended period of time, and it can decrease tolerance for dry environments, such as the air inside an airplane. Other names for dry eye include: dry eye syndrome, keratoconjunctivitis sicca (KCS), dysfunctional tear syndrome, lacrimal keratoconjunctivitis, evaporative tear deficiency, aqueous tear deficiency, and LASIK-induced neurotrophic epitheliopathy (LNE).
Types of dry eye
1) Aqueous tear-deficient dry eye is a disorder in which the lacrimal glands fail to produce enough of the watery component of tears to maintain a healthy eye surface.
2) Evaporative dry eye may result from inflammation of the meibomian glands, also located in the eyelids. These glands make the lipid or oily part of tears that slows evaporation and keeps the tears stable.
Dry eye can be associated with:
- inflammation of the surface of the eye, the lacrimal gland, or the conjunctiva;
- any disease process that alters the components of the tears;
- an increase in the surface of the eye, as in thyroid disease when the eye protrudes forward
- cosmetic surgery, if the eyelids are opened too widely.
What is the cornea?
The cornea is the clear, dome-shaped outer surface that covers the eye in front of the iris, the colored part of the eye. The cornea helps protect the rest of the eye from germs, dust, and other harmful matter. The cornea bends, or refracts, light entering the eye, and accounts for most of the eye's total focusing power. It also serves as a filter to screen out most of the damaging ultraviolet (UV) wavelengths in sunlight.
The cornea is a highly organized, clear structure made up of a group of cells and proteins precisely arranged in layers, but it has no blood vessels to nourish or protect it against infection. Instead, it receives its nourishment from the tears and the watery fluid (aqueous humor) that fills the chamber behind it.
Anatomy of the eye
What are tears, and how do they relate to dry eye?
Tears, made by the lacrimal gland, are necessary for overall eye health and clear vision. Tears bathe the surface of the eye, keeping it moist, and wash away dust and debris. They also help protect the eye from bacterial and other types of infections.
Tears are composed of three major components:
- Outer, oily, lipid layer produced by the meibomian glands
- Middle, watery, lacrimal layer produced by the lacrimal glands
- Inner, mucous or mucin layer produced by goblet cells located within a thin transparent layer over the white part of the eye and covering the inner surface of the eyelids.
Tears are made of proteins (including growth factors), electrolytes, and vitamins that are critical to maintain the health of the eye surface and to prevent infection.
Tears are constantly produced to bathe, nourish, and protect the eye surface. They are also produced in response to emergencies, such as a particle of dust in the eye, an infection or irritation of the eye, or an onset of strong emotions. When the lacrimal glands fail to produce sufficient tears, dry eye can result.
Any disease process that alters the components of tears can make them unhealthy and result in dry eye.
Dry Eye Symptoms
Dry eye symptoms may include any of the following:
- Itching, stinging or burning of the eye
- a sandy or gritty(foreign body) feeling as if something is in the eye
- episodes of excess tears following very dry eye periods
- a stringy mucus discharge from the eye
- pain and redness of the eye
- episodes of blurred vision
- heavy feeling eyelids
- inability to cry when emotionally stressed
- uncomfortable or unable to wear contact lenses
- decreased tolerance of reading, working on the computer, or any activity that requires sustained visual attention
- eye fatigue.
NOTE: If symptoms of dry eye persist, consult an eye care professional to get an accurate diagnosis of the condition and begin treatment to avoid permanent damage.
Causes and Risk Factors
What are the causes of dry eye?
Dry eye can be a temporary or chronic condition:
- Dry eye can be a side effect of some medications, including antihistamines, nasal decongestants, tranquilizers, certain blood pressure medicines, Parkinson's medications, birth control pills and anti-depressants
- skin disease on or around the eyelids can result in dry eye.
- Diseases of the glands in the eyelids, such as meibomian gland dysfunction, can cause dry eye.
- Dry eye can occur in women who are pregnant.
- Some women who are on hormone replacement therapy may experience dry eye symptoms according to one study. Women taking only estrogen were found to have a 70 percent more likely chance of developing dry eye, whereas those taking estrogen and progesterone combinations, as having a 30 percent increased risk of developing dry eye.
- Dry eye can also develop after the refractive surgery known as LASIK. These symptoms generally last three to six months, but may last longer in some cases.
- Dry eye can result from chemical and thermal burns that scar the membrane lining the eyelids and covering the eye.
- Allergies can be associated with dry eye.
- Infrequent blinking, associated with staring at computer or video screens, may also lead to dry eye symptoms.
- Both excessive and insufficient dosages of vitamins can contribute to dry eye.
- Some Homeopathic remedies may have an adverse impact on a dry eye condition.
- Loss of sensation in the cornea from long-term contact lens wear can lead to dry eye.
- Dry eye can be associated with immune system disorders such as Sjögren's syndrome, lupus, and rheumatoid arthritis. Sjögren's leads to inflammation and dryness of the mouth, eyes, and other mucous membranes. It can also affect other organs, including the kidneys, lungs and blood vessels.
- Dry eye can be a symptom of chronic inflammation of the conjunctiva, the membrane lining the eyelid and covering the front part of the eye, or the lacrimal gland. Chronic conjunctivitis can be caused by certain eye diseases, infection, exposure to irritants such as chemical fumes and tobacco smoke, or drafts from air conditioning or heating.
- If the surface area of the eye is increased, as in thyroid disease when the eye protrudes forward or after cosmetic surgery if the eyelids are opened too widely, dry eye can result.
- Dry eye may occur from exposure keratitis, in which the eyelids do not close completely during sleep.
Who is likely to develop dry eye?
Elderly people frequently experience dryness of the eyes, but dry eye can occur at any age. Nearly five million Americans 50 years of age and older are estimated to have dry eye. Of these, more than three million are women and more than one and a half million are men. Tens of millions more have less severe symptoms. Dry eye is more common after menopause. Women who experience menopause prematurely are more likely to have eye surface damage from dry eye.
Treatment
Depending on the causes of dry eye, your doctor may use various approaches to relieve the symptoms.
Dry eye can be managed as an ongoing condition. The first priority is to determine if a disease is the underlying cause of the dry eye (such as Sjögren's syndrome or lacrimal and meibomian gland dysfunction). If it is, then the underlying disease needs to be treated.
Artificial tear supplements may be used for milder cases of dry eye.
Cyclosporine, an anti-inflammatory medication, is the only prescription drug available to treat dry eye. It decreases corneal damage, increases basic tear production, and reduces symptoms of dry eye. It may take three to six months of twice-a-day dosages for the medication to work. In some cases of severe dry eye, short term use of corticosteroid eye drops that decrease inflammation is required.
If dry eye results from taking a medication, your doctor may recommend switching to a medication that does not cause the dry eye side effect.
If contact lens wear is the problem, your eye care practitioner may recommend another type of lens or reducing the number of hours you wear your lenses. In the case of severe dry eye, your eye care professional may advise you not to wear contact lenses at all.
Another option is to plug the drainage holes, small circular openings at the inner corners of the eyelids where tears drain from the eye into the nose. Lacrimal plugs, also called punctal plugs, can be inserted painlessly by an eye care professional. The patient usually does not feel them. These plugs are made of silicone or collagen, are reversible, and are a temporary measure. In severe cases, permanent plugs may be considered.
In some cases, a simple surgery, called punctal cautery, is recommended to permanently close the drainage holes. The procedure helps keep the limited volume of tears on the eye for a longer period of time.
In some patients with dry eye, supplements or dietary sources (such as tuna fish) of omega-3 fatty acids (especially DHA and EPA) may decrease symptoms of irritation. The use and dosage of nutritional supplements and vitamins should be discussed with your primary medical doctor.
What can I do to help myself?
- Use artificial tears, gels, gel inserts, and ointments - available over the counter - as the first line of therapy. They offer temporary relief and provide an important replacement of naturally produced tears in patients with aqueous tear deficiency. Avoid artificial tears with preservatives if you need to apply them more than four times a day or preparations with chemicals that cause blood vessels to constrict.
- Wearing glasses or sunglasses that fit close to the face (wrap around shades) or that have side shields can help slow tear evaporation from the eye surfaces. Indoors, an air cleaner to filter dust and other particles helps prevent dry eyes. A humidifier also may help by adding moisture to the air.
- Avoid dry conditions and allow your eyes to rest when performing activities that require you to use your eyes for long periods of time. Instill lubricating eye drops while performing these tasks.
*The National Eye Institute (NEI) is part of the National Institutes of Health (NIH) and is the Federal government's lead agency for vision research that leads to sight-saving treatments and plays a key role in reducing visual impairment and blindness.
Acute Sinusitis
Respiratory tract infections, including the common cold
and acute sinusitis, affect millions of individuals every
year. Colds are caused by viruses, are easily spread from
person to person, and are usually short-lived. Sinusitis (infection
of the paranasal sinuses) usually occurs as a result of a cold but
also can result from swelling of the nasal passages, obstruction
from a medical device or a nasal deformity, or as part of a general
infectious process in the body. Acute sinusitis may be caused by
viruses, bacteria, or, rarely, a fungus infection. Antibiotics may be
used to treat bacterial sinusitis. It is important to understand that
antibiotics do not help a cold or viral sinusitis. Using antibiotics
improperly (such as for a viral infection) can cause resistant
bacteria (that cannot be killed by the usual antibiotics) to form,
leading to antibiotic-resistant infections. 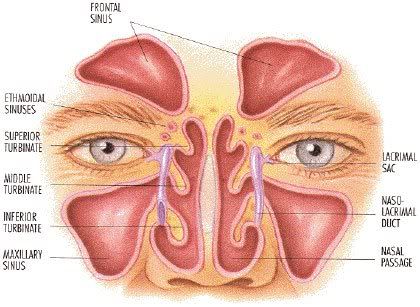
Signs and Symptoms
• Nasal obstruction
• Pain in the face over sinus areas (near
the nose, above the teeth, the forehead)
• Thick and purulent (filled with pus) nasal
discharge from both nostrils that may be
worse on one side
• Cough and sore throat (from nasal
drainage irritating the throat)
• Fatigue and feeling generally unwell
• Fever
Diagnosis
Usually the medical history and physical examination are all that is necessary to diagnose sinusitis. Sometimes x-ray studies, including computed tomography (CT) scan, may be used to confirm the diagnosis and look for causes of sinusitis. Occasionally a sample of the sinus contents (also called sinus aspiration) may be taken for laboratory examination to determine the cause.
Treatment
• Drink plenty of fluids.
• Get lots of rest and appropriate sleep.
• Inhaling steam may help to ease congestion of the sinuses.
• Temporary use of an over-the-counter nasal spray may help relieve congestion, but these should not be used for more than 5 days at a time.
• See your doctor if your symptoms last more than a few days.
• Antibiotics may be prescribed if bacterial sinusitis is suspected. It is important to take the full course of antibiotics as prescribed by your doctor. Do not skip doses or stop taking the medication when you begin to feel better.
• Seek medical attention immediately if you develop a high fever, stiff neck, severe headache, tender swelling near the eyes, or changes in your mental status such as confusion or delirium.
Sinusitis Medications
The primary goal when treating sinusitis is to decrease the inflammation in the nose and sinus openings to improve sinus drainage. This may include a combination of medical treatments. Your healthcare provider will treat an infection, if present, and try to reduce the symptoms of a runny or congested nose. Here a few recommended treatments today:
Steroid Nasal Spray
A prescription steroid nasal spray can decrease nasal inflammation and mucus production. This will decrease symptoms of nasal congestion and improve sinus drainage. A steroid nasal spray does not provide immediate relief of symptoms and may require several weeks of routine use to be effective. If you have chronic sinusitis, you may benefit from continued daily use of this medication. If you have occasional sinusitis episodes, you may only require periodic use.The combination of nasal wash and nasal steroid sprays can be highly effective for many patients with nasal and sinus problems. Several steroid nasal sprays are available and include:
Beconase AQ®,
Vancenase DS AQ® (beclomethasone)
Flonase® (fluticasone)
Nasacort AQ®,
Nasacort® (triamcinolone)
Nasarel® (flunisolide)
Nasonex® (mometasone)
Rhinocort® (budesonide )
When used properly, steroid nasal sprays are safe and effective, however, nasal dryness and bleeding are possible side effects when using these medications.
Antibiotics
Antibiotics are medicines designed to treat bacterial infections. In some cases of sinusitis, but certainly not all, the underlying cause will be a bacterial infection. Such an infection can be difficult to treat because the bacteria thrive in the warm, moist and dark areas of the sinus cavities. These infections usually respond to antibiotic treatment, however, you may need to continue treatment for one to three weeks or longer. The choice of antibiotic depends on several factors such as: drug allergies, past use of antibiotics and your symptoms. In some cases, your health care provider can collect mucus from your nose and send it to the laboratory for culture to confirm the presence of bacteria. This test can also help in the selection of the proper antibiotic to fight the infection. The majority of episodes of sinusitis (upper airway infection) are succesfully treated without the use of antibiotics by simply treating the thick mucus and nasal inflammation. Inappropriate use of antibiotics can lead to bacterial resistance and side effects, thus these medications must be used carefully and thoughtfully.
Decongestants
These medicines, available as tablet, syrup or nasal spray, help unblock the openings of the sinuses and temporarily reduce symptoms of nasal congestion. Common over the counter decongestants include Sudafed® and Dimetapp® (pseudoephedrine). Combination decongestant/antihistamine medicines are available over the counter. Read the label to see what is in the over the counter medicine you are buying and discuss the medicine with your healthcare provider. Topical nasal decongestants (sprays) can be highly effective in the immediate shrinking of swollen nasal tissue. However these sprays should be used only for 2 to 3 consecutive days because more prolonged use can cause rebound nasal congestion with increased symptoms. Systemic decongestants have the same effect of decreasing the swelling of the lining of the nose and promoting drainage of the sinuses. However, since higher concentrations are present in the bloodstream, systemic dcongestants are more likely to cause side-effects. These may include high blood pressure, anxiety, sleeplessness, prostate problems in men, and the "jitters". You should always discuss the use of these medications with your physician.
Antihistamines
Antihistamines are medicines deisgned to counter the actions of histamine, the main chemical produced in the body in allergic reactions. Antihistamines in tablet or syrup form may help reduce the allergic symptoms of sneezing, itchy eyes and nose, and may reduce mucus production. Your health care provider may elect to add this type of medicine to your treatment, particularly if allergies are present. Common over-the-counter antihistamines include:
Claritin® (loratadine)
Chlor-Trimeton (chlorpheniramine)
Benadryl (diphenhydramine)
Newer classes of prescription antihistamines do not cause drowsiness. They include:
Clarinex® (desloratadine)
Allergra® (fexofenadine)
Zyrtec® (cetirizine)
Pain Relievers
A medication to relieve pain and lessen fever may help in sinusitis, especially for acute episodes. Your healthcare provider may recommend a medication such as Tylenol® (acetaminophen), aspirin or ibuprofen, or prescribe a stronger medicine. Because some people with asthma are sensitive to aspirin or ibuprofen, check with your clinician before taking this medicine.
Systemic Steroids
Systemic steroids are sometimes required to treat severe nasal and sinus inflammation, such as nasal polyps. These medicines can be in pill or syrup form, as well as injected in a muscle or into a vein. Systemic steroids are very powerful medicines that can help nasal and sinus conditions. However, many potential side effects are possible, and include: cataract formation, high blood pressure, high blood sugar, mood changes, stomach irritation, bone loss (osteoporosis), vision change, and menstrual irregularities. These side-effects are always possible when using systemic steroids but become more of concern with longterm use. Most commonly systemic steroids will be prescribed as a pill in a "tapering" fashion. This means that your dose of steroid will be slowly decreased before completely stopping the medication. This approach also helps avoid some related complications
Headache Pain
What To Do When Your Head Hurts

Most of us get headaches from time to time. Some are mild. Others cause throbbing pain. They can last for minutes or days. There are many different types of headaches. How you treat yours depends on which kind you have.
Headaches might arise because of another medical condition, such as swollen sinuses or head injury. In these cases, treating the underlying problem usually relieves headache pain as well. But most headaches—including tension headaches and migraines—aren’t caused by a separate illness.
A headache may feel like a pain inside your brain, but it’s not. Most headaches begin in the many nerves of the muscles and blood vessels that surround your head, neck, and face. These pain-sensing nerves can be set off by stress, muscle tension, enlarged blood vessels, and other triggers. Once activated, the nerves send messages to the brain, and it can feel like the pain is coming from deep within your head.
Tension headaches are the most common type of headache. They can cause a feeling of painful pressure on the head and neck. Tension headaches occur when the muscles in your head and neck tighten, often because of stress or anxiety. Intense work, missed meals, jaw clenching, or too little sleep can bring on tension headaches.
Over-the-counter medicines such as aspirin, ibuprofen, or acetaminophen can help reduce the pain. “Lifestyle changes to relax and reduce stress might help, such as yoga, stretching, massage, and other tension relievers,” says Dr. Linda Porter, an NIH expert on pain research.
Migraines are the second-most common type of headache. They affect more than 1 in 10 people. Migraines tend to run in families and most often affect women. The pain can be severe, with pulsing and throbbing, and can last for several days. Migraine symptoms can also include blurry vision and nausea.
“Migraines are complex and can be disabling,” Porter says. Certain smells, noises, or bright flashing lights can bring on a migraine. Other triggers include lack of sleep, certain foods, skipped meals, smoking, stress, or even an approaching thunderstorm. Keeping a headache diary can help to identify the specific causes of your migraines. Avoiding those triggers or using prescription medications could help prevent or lessen the severity of future migraines.
Be careful not to overuse headache medications. Overuse can cause “rebound” headaches, making headaches more frequent and painful. People with repeating headaches, such as migraines or tension headaches, are especially at risk. Experts advise not taking certain pain-relief medicines for headaches more than 3 times a week.
A less common but more severe type of headache comes on suddenly in “clusters” at the same time of day or night for weeks. Cluster headaches may strike one side of the head, often near one eye, with a sharp or burning pain. These headaches are more common in men and in smokers.
In rare cases, a headache may warn of a serious illness. Get medical help right away if you have a headache after a blow to your head, or if you have a headache along with fever, confusion, loss of consciousness, or pain in the eye or ear.
“Know what kind of headache you have and, if you can’t manage it yourself, seek help,” Porter says. “Remember there are preventive behavioral steps and medicines that can help manage headaches. But if the pain is severe or lasting, get medical care.”
Prevent Headaches
- Ease stress.
- Get enough quality sleep.
- Eat regularly scheduled, healthy meals.
- Exercise regularly and maintain a healthy weight.
- Ask your doctor if medications might help prevent returning headaches.
**NIH News and Health nihnewsinhealth@od.nih.gov
The Sting of Shingles: Vaccine, Treatments Reduce Risks
**If you’ve ever had chickenpox, you may be at risk for a painful disease called shingles as you grow older. Shingles is a sometimes-agonizing skin rash and nerve disease that’s caused by a virus. Fortunately, you can take steps to prevent shingles or ease its serious effects.
Shingles usually affects adults after age 50, although it can strike at any age. “In the U.S., the incidence of shingles is actually increasing,” says Dr. Jeffrey Cohen, an infectious disease researcher at NIH. “If you live to be 85 years old, you have a 50% chance of getting shingles.”
Shingles is caused by the varicella-zoster virus—the same virus that causes chickenpox. Once you’ve had chickenpox, the virus stays with you for life, hidden and inactive in your nerve cells. Your immune system helps keep chickenpox from returning. But later in life, the virus can re-emerge and cause shingles (also known as herpes zoster).
You can’t “catch” shingles from someone else. But it is possible for a person with a blistery shingles rash to pass on the varicella-zoster virus to someone who’s never had chickenpox or a chickenpox vaccine. If that happens, the other person would get chickenpox, not shingles.
Shingles may cause skin sensitivity ranging from mild itching to severe pain along with burning, tingling, or numbness. A rash with fluid-filled blisters nearly always appears on just one side of the body or face. The rash usually lasts for 7 to 10 days. Other symptoms may include chills, fever, upset stomach, and headache.
Shingles can lead to some serious problems. If it appears on your face, it can affect your hearing and vision. It may cause lasting eye damage or blindness. After the rash fades, the pain may linger for months or years, especially in older people. This lasting pain, called post-herpetic neuralgia, affects nearly 1 out of every 3 older people with shingles. The pain can be so severe that even the gentlest touch or breeze can feel excruciating.
To help prevent these problems, see your doctor at the first sign of shingles. Early treatment can shorten the length of infection and reduce the risk of serious complications.
To treat shingles, your doctor may prescribe antiviral drugs to help fight the varicella-zoster virus. Steroids can lessen pain and shorten the time you’re sick. Other types of medicines can also relieve pain.
Fortunately, a vaccine called Zostavax can help prevent shingles or decrease its severity. It’s been approved by the U.S. Food and Drug Administration (FDA) for people ages 50 and older. “The vaccine can prevent shingles and reduce the risk of post-herpetic neuralgia, which can be very debilitating,” Cohen says.
The shingles vaccine is available by prescription. Unfortunately, the vaccine is expensive, and the costs aren’t always covered by health insurance. If you’re considering the shingles vaccine, be sure to discuss the pros and cons of the vaccine with your doctor, and check with your insurance provider about coverage.
Now that people have been receiving the shingles vaccine for several years, researchers are evaluating whether booster shots might be appropriate. Scientists are also studying post-herpetic neuralgia to find better ways to treat this complication from shingles.
**NIH News and Health nihnewsinhealth@od.nih.gov
Kidney Stones (nephrolithiasis)
History
Kidney stones, one of the most painful of the urologic disorders, have beset humans for centuries. Scientists have found evidence of kidney stones in a 7,000-year-old Egyptian mummy. Unfortunately, kidney stones are one of the most common disorders of the urinary tract. Each year, people make almost 3 million visits to health care providers and more than half a million people go to emergency rooms for kidney stone problems.
Most kidney stones pass out of the body without any intervention by a physician. Stones that cause lasting symptoms or other complications may be treated by various techniques, most of which do not involve major surgery. Also, research advances have led to a better understanding of the many factors that promote stone formation and thus better treatments for preventing stones.
Introduction to the Urinary Tract
The urinary tract, or system, consists of the kidneys, ureters, bladder, and urethra. The kidneys are two bean-shaped organs located below the ribs toward the middle of the back, one on each side of the spine. The kidneys remove extra water and wastes from the blood, producing urine. They also keep a stable balance of salts and other substances in the blood. The kidneys produce hormones that help build strong bones and form red blood cells.
Narrow tubes called ureters carry urine from the kidneys to the bladder, an oval-shaped chamber in the lower abdomen. Like a balloon, the bladder's elastic walls stretch and expand to store urine. They flatten together when urine is emptied through the urethra to outside the body.
What is a kidney stone?
A kidney stone is a hard mass developed from crystals that separate from the urine within the urinary tract. Normally, urine contains chemicals that prevent or inhibit the crystals from forming. These inhibitors do not seem to work for everyone, however, so some people form stones. If the crystals remain tiny enough, they will travel through the urinary tract and pass out of the body in the urine without being noticed.
Kidney stones may contain various combinations of chemicals.
The most common type of stone contains calcium in combination with either oxalate or phosphate. These chemicals are part of a person's normal diet and make up important parts of the body, such as bones and muscles.
A less common type of stone is caused by infection in the urinary tract. This type of stone is called a struvite or infection stone. Another type of stone, uric acid stones, are a bit less common, and cystine stones are rare.
Urolithiasis is the medical term used to describe stones occurring in the urinary tract. Other frequently used terms are urinary tract stone disease and nephrolithiasis. Doctors also use terms that describe the location of the stone in the urinary tract. For example, a ureteral stone-or ureterolithiasis-is a kidney stone found in the ureter. To keep things simple, the general term kidney stones is used throughout this fact sheet.
Gallstones and kidney stones are not related. They form in different areas of the body. Someone with a gallstone is not necessarily more likely to develop kidney stones.
Who gets kidney stones?
For unknown reasons, the number of people in the United States with kidney stones has been increasing over the past 30 years. In the late 1970s, less than 4 percent of the population had stone-forming disease. By the early 1990s, the portion of the population with the disease had increased to more than 5 percent.
Caucasians are more prone to develop kidney stones than African Americans. Stones occur more frequently in men. The prevalence of kidney stones rises dramatically as men enter their 40s and continues to rise into their 70s. For women, the prevalence of kidney stones peaks in their 50s. Once a person gets more than one stone, other stones are likely to develop.
What causes kidney stones?
Doctors do not always know what causes a stone to form. While certain foods may promote stone formation in people who are susceptible, scientists do not believe that eating any specific food causes stones to form in people who are not susceptible.
A person with a family history of kidney stones may be more likely to develop stones. Urinary tract infections, kidney disorders such as cystic kidney diseases, and certain metabolic disorders such as hyperparathyroidism are also linked to stone formation.
In addition, more than 70 percent of people with a rare hereditary disease called renal tubular acidosis develop kidney stones.
Cystinuria and hyperoxaluria are two other rare, inherited metabolic disorders that often cause kidney stones. In cystinuria, too much of the amino acid cystine, which does not dissolve in urine, is voided, leading to the formation of stones made of cystine. In patients with hyperoxaluria, the body produces too much oxalate, a salt. When the urine contains more oxalate than can be dissolved, the crystals settle out and form stones.
Hypercalciuria is inherited, and it may be the cause of stones in more than half of patients. Calcium is absorbed from food in excess and is lost into the urine. This high level of calcium in the urine causes crystals of calcium oxalate or calcium phosphate to form in the kidneys or elsewhere in the urinary tract.
Other causes of kidney stones are hyperuricosuria, which is a disorder of uric acid metabolism; gout; excess intake of vitamin D; urinary tract infections; and blockage of the urinary tract. Certain diuretics, commonly called water pills, and calcium-based antacids may increase the risk of forming kidney stones by increasing the amount of calcium in the urine.
Calcium oxalate stones may also form in people who have chronic inflammation of the bowel or who have had an intestinal bypass operation, or ostomy surgery. As mentioned earlier, struvite stones can form in people who have had a urinary tract infection. People who take the protease inhibitor indinavir, a medicine used to treat HIV infection, may also be at increased risk of developing kidney stones.
Foods and Drinks Containing Oxalate
People prone to forming calcium oxalate stones may be asked by their doctor to limit or avoid certain foods if their urine contains an excess of oxalate.
High-oxalate foods-higher to lower
- rhubarb
- spinach
- beets
- swiss chard
- wheat germ
- soybean crackers
- peanuts
- okra
- chocolate
- black Indian tea
- sweet potatoes
Foods that have medium amounts of oxalate may be eaten in limited amounts.
Medium-oxalate foods-higher to lower
- grits
- grapes
- celery
- green pepper
- red raspberries
- fruit cake
- strawberries
- marmalade
- liver
Source: The Oxalosis and Hyperoxaluria Foundation
What are the symptoms of kidney stones?
Kidney stones often do not cause any symptoms. Usually, the first symptom of a kidney stone is extreme pain, which begins suddenly when a stone moves in the urinary tract and blocks the flow of urine. Typically, a person feels a sharp, cramping pain in the back and side in the area of the kidney or in the lower abdomen. Sometimes nausea and vomiting occur. Later, pain may spread to the groin.
If the stone is too large to pass easily, pain continues as the muscles in the wall of the narrow ureter try to squeeze the stone into the bladder. As the stone moves and the body tries to push it out, blood may appear in the urine, making the urine pink. As the stone moves down the ureter, closer to the bladder, a person may feel the need to urinate more often or feel a burning sensation during urination.
If fever and chills accompany any of these symptoms, an infection may be present. In this case, a person should contact a doctor immediately.
How are kidney stones diagnosed?
Sometimes "silent" stones-those that do not cause symptoms-are found on x rays taken during a general health exam. If the stones are small, they will often pass out of the body unnoticed. Often, kidney stones are found on an x ray or ultrasound taken of someone who complains of blood in the urine or sudden pain. These diagnostic images give the doctor valuable information about the stone's size and location. Blood and urine tests help detect any abnormal substance that might promote stone formation.
The doctor may decide to scan the urinary system using a special test called a computerized tomography (CT) scan or an intravenous pyelogram (IVP). The results of all these tests help determine the proper treatment.
Preventing Kidney Stones
A person who has had more than one kidney stone may be likely to form another; so, if possible, prevention is important. To help determine their cause, the doctor will order laboratory tests, including urine and blood tests. The doctor will also ask about the patient's medical history, occupation, and eating habits. If a stone has been removed, or if the patient has passed a stone and saved it, a stone analysis by the laboratory may help the doctor in planning treatment.
The doctor may ask the patient to collect urine for 24 hours after a stone has passed or been removed. For a 24-hour urine collection, the patient is given a large container, which is to be refrigerated between trips to the bathroom. The collection is used to measure urine volume and levels of acidity, calcium, sodium, uric acid, oxalate, citrate, and creatinine-a product of muscle metabolism. The doctor will use this information to determine the cause of the stone. A second 24-hour urine collection may be needed to determine whether the prescribed treatment is working.
How are kidney stones treated?
Fortunately, surgery is not usually necessary. Most kidney stones can pass through the urinary system with plenty of water-2 to 3 quarts a day-to help move the stone along. Often, the patient can stay home during this process, drinking fluids and taking pain medication as needed. The doctor usually asks the patient to save the passed stone(s) for testing. It can be caught in a cup or tea strainer used only for this purpose.
Lifestyle Changes
A simple and most important lifestyle change to prevent stones is to drink more liquids-water is best. Someone who tends to form stones should try to drink enough liquids throughout the day to produce at least 2 quarts of urine in every 24-hour period.
In the past, people who form calcium stones were told to avoid dairy products and other foods with high calcium content. Recent studies have shown that foods high in calcium, including dairy products, may help prevent calcium stones. Taking calcium in pill form, however, may increase the risk of developing stones.
Patients may be told to avoid food with added vitamin D and certain types of antacids that have a calcium base. Someone who has highly acidic urine may need to eat less meat, fish, and poultry. These foods increase the amount of acid in the urine.
To prevent cystine stones, a person should drink enough water each day to dilute the concentration of cystine that escapes into the urine, which may be difficult. More than a gallon of water may be needed every 24 hours, and a third of that must be drunk during the night.
Medical Therapy
A doctor may prescribe certain medications to help prevent calcium and uric acid stones. These medicines control the amount of acid or alkali in the urine, key factors in crystal formation. The medicine allopurinol may also be useful in some cases of hyperuricosuria.
Doctors usually try to control hypercalciuria, and thus prevent calcium stones, by prescribing certain diuretics, such as hydrochlorothiazide. These medicines decrease the amount of calcium released by the kidneys into the urine by favoring calcium retention in bone. They work best when sodium intake is low.
Rarely, patients with hypercalciuria are given the medicine sodium cellulose phosphate, which binds calcium in the intestines and prevents it from leaking into the urine.
If cystine stones cannot be controlled by drinking more fluids, a doctor may prescribe medicines such as Thiola and Cuprimine, which help reduce the amount of cystine in the urine.
For struvite stones that have been totally removed, the first line of prevention is to keep the urine free of bacteria that can cause infection. A patient's urine will be tested regularly to ensure no bacteria are present.
If struvite stones cannot be removed, a doctor may prescribe a medicine called acetohydroxamic acid (AHA). AHA is used with long-term antibiotic medicines to prevent the infection that leads to stone growth.
People with hyperparathyroidism sometimes develop calcium stones. Treatment in these cases is usually surgery to remove the parathyroid glands, which are located in the neck. In most cases, only one of the glands is enlarged. Removing the glands cures the patient's problem with hyperparathyroidism and kidney stones.
Surgical Treatment
Surgery may be needed to remove a kidney stone if it:
- does not pass after a reasonable period of time and causes constant pain
- is too large to pass on its own or is caught in a difficult place
- blocks the flow of urine
- causes an ongoing urinary tract infection
- damages kidney tissue or causes constant bleeding
- has grown larger, as seen on follow-up x rays
Until 20 years ago, open surgery was necessary to remove a stone. The surgery required a recovery time of 4 to 6 weeks. Today, treatment for these stones is greatly improved, and many options do not require major open surgery and can be performed in an outpatient setting.
Extracorporeal Shock Wave Lithotripsy
Extracorporeal shock wave lithotripsy (ESWL) is the most frequently used procedure for the treatment of kidney stones. In ESWL, shock waves that are created outside the body travel through the skin and body tissues until they hit the denser stones. The stones break down into small particles and are easily passed through the urinary tract in the urine.
Several types of ESWL devices exist. Most devices use either x rays or ultrasound to help the surgeon pinpoint the stone during treatment. For most types of ESWL procedures, anesthesia is needed.
In many cases, ESWL may be done on an outpatient basis. Recovery time is relatively short, and most people can resume normal activities in a few days.
Complications may occur with ESWL. Some patients have blood in their urine for a few days after treatment. Bruising and minor discomfort in the back or abdomen from the shock waves can occur. To reduce the risk of complications, doctors usually tell patients to avoid taking aspirin and other medicines that affect blood clotting for several weeks before treatment.
Sometimes, the shattered stone particles cause minor blockage as they pass through the urinary tract and cause discomfort. In some cases, the doctor will insert a small tube called a stent through the bladder into the ureter to help the fragments pass. Sometimes the stone is not completely shattered with one treatment, and additional treatments may be needed.
As with any interventional, surgical procedure, potential risks and complications should be discussed with the doctor before making a treatment decision.
Percutaneous Nephrolithotomy
Sometimes a procedure called percutaneous nephrolithotomy is recommended to remove a stone. This treatment is often used when the stone is quite large or in a location that does not allow effective use of ESWL.
In this procedure, the surgeon makes a tiny incision in the back and creates a tunnel directly into the kidney. Using an instrument called a nephroscope, the surgeon locates and removes the stone. For large stones, some type of energy probe-ultrasonic or electrohydraulic-may be needed to break the stone into small pieces. Often, patients stay in the hospital for several days and may have a small tube called a nephrostomy tube left in the kidney during the healing process.
One advantage of percutaneous nephrolithotomy is that the surgeon can remove some of the stone fragments directly instead of relying solely on their natural passage from the kidney.
Ureteroscopic Stone Removal
Although some stones in the ureters can be treated with ESWL, ureteroscopy may be needed for mid- and lower-ureter stones. No incision is made in this procedure. Instead, the surgeon passes a small fiberoptic instrument called a ureteroscope through the urethra and bladder into the ureter. The surgeon then locates the stone and either removes it with a cage-like device or shatters it with a special instrument that produces a form of shock wave. A small tube or stent may be left in the ureter for a few days to help urine flow. Before fiber optics made ureteroscopy possible, physicians used a similar "blind basket" extraction method. But this technique is rarely used now because of the higher risks of damage to the ureters.
Research
The Division of Kidney, Urologic, and Hematologic Diseases of the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) funds research on the causes, treatments, and prevention of kidney stones. The NIDDK is part of the National Institutes of Health in Bethesda, MD.
New medicines and the growing field of lithotripsy have greatly improved the treatment of kidney stones. Still, NIDDK researchers and grantees seek to answer questions such as
- Why do some people continue to have painful stones?
- How can doctors predict, or screen, those at risk for getting stones?
- What are the long-term effects of lithotripsy?
- Do genes play a role in stone formation?
- What is the natural substance(s) found in urine that blocks stone formation?
Researchers are also developing new medicines with fewer side effects.
Points to Remember
- A person with a family history of stones or a personal history of more than one stone may be more likely to develop more stones.
- A good first step to prevent the formation of any type of stone is to drink plenty of liquids-water is best.
- Someone who is at risk for developing stones may need certain blood and urine tests to determine which factors can best be altered to reduce that risk.
- Some people will need medicines to prevent stones from forming.
- People with chronic urinary tract infections and stones will often need a stone removed if the doctor determines that the stone is causing the infection. Patients must receive careful follow-up to be sure that the infection has cleared.
**Note: We do not endorse or favor any specific commercial product or company. Trade, proprietary, or company names appearing in this document are used only because they are considered necessary in the context of the information provided. If a product is not mentioned, the omission does not mean or imply that the product is unsatisfactory.
American Urological Association Foundation
1000 Corporate Boulevard
Linthicum, MD 21090
Phone: 1-866-RING-AUA (746-4282) or 410-689-3700
Email: patienteducation@auafoundation.org
Internet: www.auafoundation.org
www.UrologyHealth.org
National Kidney Foundation
30 East 33rd Street
New York, NY 10016
Phone: 1-800-622-9010 or 212-889-2210
Internet: www.kidney.org
Oxalosis and Hyperoxaluria Foundation
201 East 19th Street, Suite 12E
New York, NY 10003
Phone: 1-800-OHF-8699 (643-8699) or 212-777-0470
Fax: 212-777-0471
Email: execdirector@ohf.org
Internet: www.ohf.org
For Information About Hyperparathyroidism:
National Endocrine and Metabolic Diseases Information Service
National Institute of Diabetes and Digestive and Kidney Diseases
National Institutes of Health
6 Information Way
Bethesda, MD 20892-3569
Phone: 1-888-828-0904
Fax: 703-738-4929
Email: endoandmeta@info.niddk.nih.gov
For Information About Gout:
National Institute of Arthritis and Musculoskeletal and Skin Diseases Information Clearinghouse
National Institutes of Health
1 AMS Circle
Bethesda, MD 20892-3675
Phone: 1-877-22-NIAMS (226-4267) or 301-495-4484
TTY: 301-565-2966
Fax: 301-718-6366
Email: niamsinfo@mail.nih.gov
Internet: www.niams.nih.gov
Allergy Season and the Eye: Allergic Conjunctivitis
Allergic conjunctivitis is inflammation of the tissue lining the eyelids (conjunctiva) due to a reaction from allergy-causing substances such as pollen and dander.
Symptoms may be seasonal and can include:
- Red eyes
- Dilated vessels in the clear tissue covering white of the eye
- Intense itching or burning eyes
- Puffy eyelids, especially in the morning
- Tearing (watery eyes)
- Stringy eye discharge
The pollens that cause symptoms vary from person to person and from area to area. Tiny, hard-to-see pollens that may cause hay fever include:
- Grasses
- Ragweed
- Trees
The amount of pollen in the air can affect whether you develop symptoms. There is more likely to be increased amounts of pollen in the air on hot, dry, windy days. On cool, damp, rainy days most pollen is washed to the ground.
The best treatment is to avoid what causes your allergy symptoms. It may be very difficult to avoid all of your triggers. However, you can often take steps to reduce your exposure to triggers such as:
- Dust
- Mold
- Pollen
Lubricating eye drops can help decrease symptoms and you can relieve discomfort by applying cool compresses to the eyes. Over-the-counter oral antihistamines can provide more relief. However, they can sometimes make the eyes dry.
If home-care measures do not help, treatment by your health care provider may be necessary, which may include:
- Antihistamine or anti-inflammatory drops that are placed into the eye
- Mild eye steroid preparations applied directly on the surface of the eye (for severe reactions)
- Eye drops that prevent certain white blood cells called mast cells from releasing histamine; these drops are given in combination with antihistamines for moderate to severe reactions
When your eyes are exposed to anything to which you are allergic, histamine is released and the blood vessels in the conjunctiva become swollen (the conjunctiva is the clear membrane that covers the "white" of the eye). Reddening of the eyes develops quickly and is accompanied by itching and tearing.
Allergies tend to run in families, although no obvious mode of inheritance is recognized. The incidence of allergy is difficult to determine, because many different conditions are often lumped under the term allergy. Rubbing the eyes generally makes the situation worse.
Your doctor may look for the following:
- Certain white blood cells, called eosinophils, in scrapings, secretions, or discharge
- Small, raised bumps on the inside of the eyelids (papillary conjunctivitis)
- Positive skin test for suspected allergens
Treatment usually relieves the symptoms. However, the condition tends to recur if exposure to the offending agent continues.
Prevention of allergic conjunctivitis is best accomplished by avoiding the allergen, if it is known. In many cases, however, this is impossible since the allergy-causing agents are everywhere nearly all the time.
There are usually no serious complications, and persistent discomfort is common.
If you experience allergic conjunctivitis and it is unresponsive to over-the-counter treatment, you should see your health care provider for an evaluation and management.
*National Library of Medicine
Red, Itchy Rash?
Get the Skinny on Dermatitis

You’ve probably had a rash at some point or another, whether from poison ivy or the chickenpox or something more unusual. Why does your skin break out in red blotches like that? More important, is there anything you can do about it?
We often think of the skin as a barrier—it keeps the insides of our bodies in, and it keeps the outside world out. But our skin is also filled with special cells of the immune system. These cells protect the skin and body against viruses, bacteria and other threats. Whenever these cells detect a suspicious substance, they begin a chain reaction in the skin that leads to inflammation. The medical name for this reaction is dermatitis. But it’s more commonly known as a rash.
There are many different types of dermatitis, and each has a distinct set of treatments. Sometimes the skin’s immune cells react to something that directly touches the skin. Other times, the immune system flares in the skin because of a whole-body infection or illness.
The symptoms of these different types of rashes often overlap. “Itching is a common symptom for all these problems,” says Dr. Stephen I. Katz, director of NIH’s National Institute of Arthritis and Musculoskeletal and Skin Diseases. Many rashes are red, painful, and irritated. Some types of rash can also lead to blisters or patches of raw skin. While most rashes clear up fairly quickly, others are long lasting and need to be cared for over long periods of time.
Eczema, or atopic dermatitis, is a dry, red, itchy rash that affects up to 1 in 5 infants and young children. It often improves over time, although it can last into adulthood or start later in life. In this condition, the water-tight barrier between skin cells gets weak, which lets moisture out and other things in. That’s why people with atopic dermatitis have to moisturize their skin, and they’re more susceptible to skin infections.
Researchers have recently identified specific genes that are involved in maintaining the skin barrier. People with certain versions of these genes are more likely to get atopic dermatitis.
“The skin is the outermost sentinel for fighting off bacteria and noxious agents,” says Katz. “If the barrier is broken somehow, you can become more allergic to things.”
A skin allergy, or allergic contact dermatitis, produces a red, itchy rash that sometimes comes with small blisters or bumps. The rash arises when the skin comes in contact with an allergen, a usually harmless substance that the immune system attacks. Allergens trigger allergic reactions. Allergens can come from certain soaps, creams and even pets.
Your immune system might not react the first time you encounter an allergen. But over time, your immune system can become sensitive to the substance. As a result, your next contact may lead to inflammation and an allergic rash.
“The most common form of dermatitis that is seen anywhere is an allergic contact dermatitis to nickel,” says Katz. “Why? Because of ear piercing.” Many inexpensive earrings are made of nickel, and over time, wearing nickel earrings can cause an allergic reaction to the metal.
Other common causes of allergic dermatitis are poison oak and poison ivy. The stems and leaves of these plants produce a chemical that’s likely to cause allergies. If you touch one of them, wash your skin as soon as possible. The chemical can also remain in clothing for a long time, so it’s important to wash any clothes or shoes—or even pets—that come into contact with these plants.
Mild cases of allergic contact dermatitis usually disappear after a few days or weeks. But if the rash persists, is extremely uncomfortable or occurs on the face, it’s important to see a physician. A doctor can prescribe medications that will tone down the immune reaction in the skin. This eases swelling and itching and will protect your eyes and face.
The immune cells of the skin can also produce rashes when they react to invading germs—like bacteria, fungi and viruses. Bacterial and viral infections within your body can cause your skin to break out in spots as well. The chickenpox virus, for example, can cause itchy spots in children. Years later, in older adults, the same virus may reappear as shingles, bringing a painful rash and high fever. Vaccines can prevent several rash-causing diseases, including chickenpox, shingles and measles.
Certain drugs, including antibiotics like amoxicillin, may also cause itchy skin rashes. If you’re allergic to a drug, a rash can be the first sign of a serious reaction. As with other allergies, a reaction to a drug may not occur the first time you take it. It could show up after several uses. Not all drug rashes are due to an allergy, however. If you break out in itchy spots after starting a new drug prescription, contact your doctor right away.
While most rashes get better with time, some can last a lifetime. Psoriasis, a condition where skin cells build up into thick red patches, tends to run in families. “It’s a complex genetic disease, in that there’s not one gene that causes psoriasis but many,” says Katz. Even though none of these genes alone has a great effect on the disease, knowing which genes are involved can help researchers design potential new treatments. Other long-term diseases that can produce rashes include autoimmune diseases, such as lupus, and some forms of cancer.
If you notice an itchy or painful rash on your skin, think twice before going to the drugstore and getting some cream if you don’t know the cause. “The creams that you buy can produce problems that make your original problem even worse,” Katz says. Because rashes can be caused by many different things—bacteria, viruses, drugs, allergies, genetic disorders, and even light—it’s important to figure out what kind of dermatitis you have.
“If you have any significant rash, you should see a dermatologist,” says Katz. A dermatologist, or skin doctor, is specially trained to figure out what’s causing a rash and help you get the right treatment.
Your skin is your protection. It’s not just the covering that keeps your body in; it’s also your first line of defense against germs and chemicals. Take care of your skin so your skin can take care of you.
*NIH News in Health
*This is a medical informational site only and and should be treated as such. It is not intended for self diagnosis and treatment which is not implied nor its purpose. This site is only providing general information on certain medical conditions for educational purposes only. If you have any medical conditions or concerns, you should always see your medical provider for a proper and thorough clinical work-up and evaluation. We do not endorse or favor any specific commercial product or company. Trade, proprietary, or company names appearing in this document are used only because they are considered necessary in the context of the information provided. If a product is not mentioned, the omission does not mean or imply that the product is unsatisfactory.
Copyright (c) 2020-2021 G.Bennett M.D.